Focus is on inhibiting action of myeloid-derived suppressor cells
Glioblastoma (GBM) is notorious for evading traditional treatments for advanced cancers, some of which are aligned toward activating T cells via immune checkpoint inhibition. These strategies have not been consistently successful in GBM, likely due to abundant immunosuppressive mechanisms that counteract T cell activation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Now a Cleveland Clinic-led team is pursuing research to elucidate the mechanisms of immunosuppression that enable GBM to evade traditional treatment. Their work received a recent boost from a five-year, $2.1 million grant from the National Institute of Neurological Disorders and Stroke (NINDS). “Our ultimate aim is to develop new therapies to overcome GBM’s therapeutic resistance,” says principal investigator Justin Lathia, PhD, Vice Chair of the Department of Cardiovascular and Metabolic Sciences in Cleveland Clinic’s Lerner Research Institute. The project is being co-led by Michael Vogelbaum, MD, PhD, a neurosurgeon at Moffitt Cancer Center in Tampa, Florida.
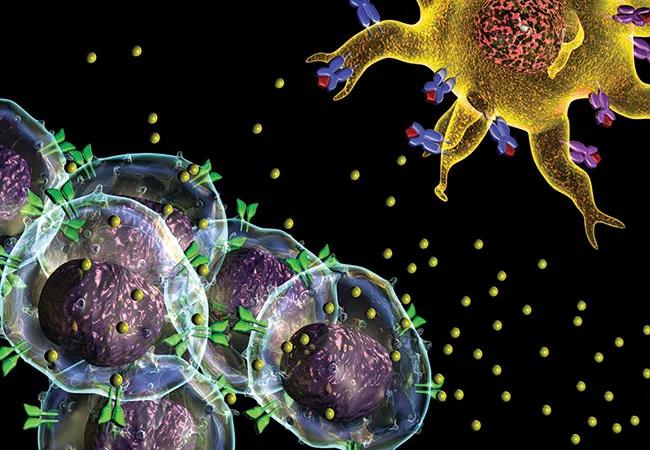
While most GBM treatments target tumor cells, Dr. Lathia and his team seek to inhibit the activity of immunosuppressive cells known as myeloid-derived suppressor cells (MDSCs) to reduce tumor growth.
Their current research builds on previous work by Dr. Lathia and Dr. Vogelbaum showing that MDSC levels are elevated in GBM patients with particularly poor prognosis. It is believed that GBM tumors secrete factors that promote migration of MDSCs to the brain. Upon migration, a complex signaling cascade, which involves cancer stem cells and macrophage migration inhibitory factor (MIF), activates the MDSCs. When activated, MDSCs block the beneficial antitumor immune response, allowing tumors to grow and spread unchecked.
With the new award from the NINDS, the team will study how these various cells work and evaluate the therapeutic benefit of targeting intratumoral MDSCs. They will explore whether novel MIF-targeting therapies can effectively slow GBM growth by reversing the mechanisms by which MDSCs suppress the immune system.
Advertisement
“In view of the high number of immunosuppressive MDSCs present in glioblastoma, activating T cells alone may not be adequate to attenuate tumor growth,” explains Dr. Lathia. “Yet there may be an opportunity to generate a durable immune response by concurrently activating T cells while also inhibiting MDSCs.”
He adds that understanding of how the immune system operates in the brain in both normal and pathological conditions is improving. “This knowledge should help us target these infiltrating cell populations as alternative therapies to encourage patients’ own immune systems to successfully attack glioblastoma tumors,” he notes.
Advertisement
Advertisement

First full characterization of kidney microbiome unlocks potential to prevent kidney stones

Researchers identify potential path to retaining chemo sensitivity

Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests

Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology