Pain, quality of life and other patient-reported data are significantly improved one year after surgery

By Georgeanne Botek, DPM, and Sara Lyn Miniaci-Coxhead, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Great toe pain is one of the most common complaints in patients presenting to a foot and ankle clinic. Approximately one in five people over the age of 50 will experience a bunion (hallux valgus) or arthritis of the first metatarsophalangeal (MTP) joint (hallux rigidus). With adults living longer and being more physically active into their 70s, complaints of painful arthritis and bunions will only increase.
Fusion is the most popular way to address end-stage deformities and arthritis of the first MTP joint. It is the gold standard for treating late stages of hallux rigidus, arthritic hallux valgus, geriatric hallux valgus, revision first ray surgeries and inflammatory arthropathies such as rheumatoid arthritis. It affords predictable pain relief, offers position maintenance, restores foot function and may provide good long-term outcomes compared to other surgical procedures. A review of the literature shows good to excellent outcomes across the board. Almost all studies report a greater than 90% fusion rate, with patient satisfaction greater than 80%.
The Outcomes Management and Evaluation (OME) system is a database of information prospectively collected for almost all orthopaedic procedures performed at Cleveland Clinic. Patients are enrolled on the day of surgery, when complete patient-reported outcome measures (PROMs) are collected along with surgeon-reported information about the specific procedure. PROMs also are collected six months and one year after surgery.
In 2016, we began collecting data on first MTP joint fusions. The database includes multiple surgeons (podiatrists and orthopaedic surgeons) and locations throughout Cleveland Clinic’s health system in Northeast Ohio.
Advertisement
Between August 2016 and May 2021, 756 patients underwent a first MTP joint fusion at our institution. Of these, we reviewed 406 (54%) patients who had a complete dataset (baseline PROMs, surgeon data and one-year PROMs). Our patient cohort included 317 women (78%), with an average age of 65 (age range: 54-71). Indications for surgery included hallux rigidus (N = 117), hallux valgus (N = 135), arthritic bunion (N = 116), hallux varus (N = 19) and other (N = 19).
The baseline Veterans RAND 12-Item Health Survey (VR-12) for physical health was 36.8 versus 43.3 at one year (P < .001), while the VR-12 for mental health remained similar at 53.4 to 52.7 (P = .115). All Foot and Ankle Outcome Score (FAOS) subscores (for pain, symptoms, activities of daily living [ADLs], sports/recreation and quality of life) had a statistically significant increase from baseline to one year after surgery.
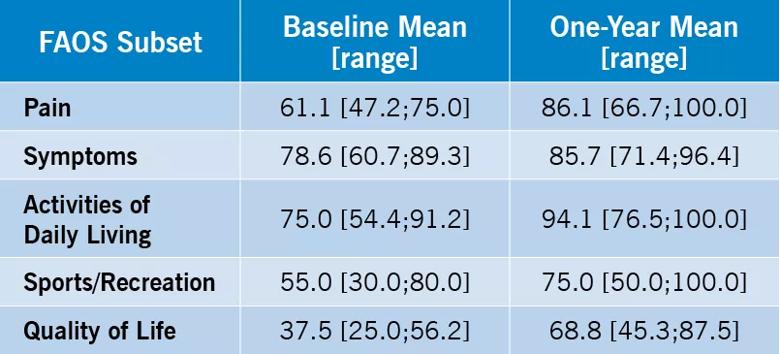
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6e03e926-6483-43bc-9a66-f70ad6c3f48d/22-ORI-3184567-CQD-Inset-Table_jpg)
Overall, patients do well after first MTP joint fusion and are happy with their results, as demonstrated in these two cases.
A healthy 52-year-old fitness instructor presented with bilateral hallux rigidus (Figure 1). She initially underwent arthrodesis of the left great toe. Two years later, the contralateral fusion was elected. Now she is at full unrestricted physical activity and pain-free with bilateral first MTP joint fusions (Figures 2-4).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5bd2b14f-0f75-444f-ae80-27c51bec37ea/22-ORI-3184567-CQD-Inset1_jpg)
Figure 1. Preoperative radiograph of bilateral hallux rigidus.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d8891d8d-390d-4620-86a8-e3a5bfb58675/22-ORI-3184567-CQD-Inset2_jpg)
Figure 2. Anterior-to-posterior radiograph three years after left fusion and one year after right fusion.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/361792df-0f76-4134-ad33-366c61d36de7/22-ORI-3184567-CQD-Inset3_jpg)
Figure 3. Postoperative lateral radiograph of left fusion.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e9cae0e2-2a7d-4e7c-9ff5-02f080bb1783/22-ORI-3184567-CQD-Inset4_jpg)
Figure 4. Postoperative lateral radiograph of right fusion.
A healthy 75-year-old female presented with bilateral great toe pain, worse on the left foot than the right (Figure 5). She reported that the pain was interfering with her ADLs, including walking for exercise. At four months after first MTP joint fusion on the left foot, she had no pain and had returned to all activities (Figures 6 and 7).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b22287bd-7feb-4cdd-8f5d-0d09e5192462/22-ORI-3184567-CQD-Inset5_jpg)
Figure 5. Anterior-to-posterior radiograph of patient with bilateral great toe pain.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9d5dc74d-613f-435b-872c-7dbf507eb199/22-ORI-3184567-CQD-Inset6-597x1024_jpg)
Figure 6. Oblique radiograph after left fusion.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/35edcbca-d81e-485e-a349-e0417ec9d22d/22-ORI-3184567-CQD-Inset7_jpg)
Figure 7. Lateral radiograph after left fusion.
In conclusion, first MTP joint fusion is a reliable procedure that produces favorable outcomes in patients with various first MTP ailments. Our prospectively collected data have demonstrated that the surgery is successful across multiple locations, surgeons and diagnoses. Although implants for arthroplasty of the first MTP joint now are available, outcomes of first MTP fusion consistently are superior.
Dr. Botek is Head of Podiatry within Cleveland Clinic’s Foot & Ankle Center. Dr. Miniaci-Coxhead is an orthopaedic surgeon in the Foot & Ankle Center, with a joint appointment in Cleveland Clinic’s Sports Medicine Center.
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians

Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Percutaneous stabilization can increase mobility without disrupting cancer treatment