Criteria include spinal curve less than 65 degrees, remaining skeletal growth
Vertebral body tethering (VBT) is a relatively new technique for treating progressive scoliosis in children. Instead of conventional spinal fusion surgery, which significantly reduces spinal mobility, VBT preserves mobility while guiding the spine into alignment as a child grows.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The surgical treatment has been offered at Cleveland Clinic since 2019.
“The idea behind VBT is much like growth modulation used in limb correction, which many pediatricians may already know,” explains Cleveland Clinic pediatric spine surgeon Kevin Serdahely, MD. “In growth modulation, or ‘guided growth,’ we attach a device near a growth center in a child’s leg to help it straighten as it grows. VBT applies this same principle to the spine. We place forces on one side of the spine’s growth centers so the other side can catch up.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d5872314-6261-4623-8784-e4e0671edcdf/25-ORI-6530659CQD-Pediatric-spine-growth-modulation)
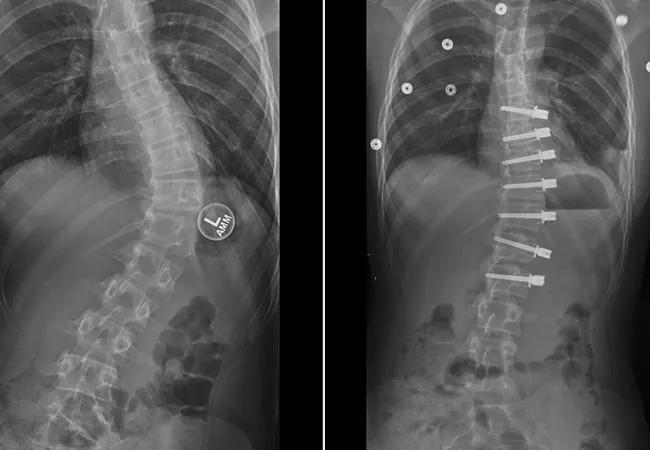
Progression of scoliosis correction with VBT. A. Spinal curve in a 13-year-old patient with idiopathic scoliosis. B. Initial radiograph after VBT surgery, displaying partial correction of the curve. C. Continuing correction of the spinal curve six months after surgery. D. Further correction of the spinal curve 18 months after surgery.
Unlike spinal fusion, which requires a large incision on the patient’s back, VBT is minimally invasive, performed through tiny incisions on one side of the child’s chest.
The anesthesia team positions the patient on their side (convex spinal curve up) and then selectively deflates one lung to facilitate visualization of the front of the spine. Screw-like devices are inserted into each vertebra on the convex side of the curved spine. The screws then are tethered together with a flexible cord.
The tension of the cord applies force to the patient’s spinal growth centers, causing them to grow slower so the untethered (concave) side of the spine can catch up as it grows normally — usually over 12-24 months. The cord usually does not need to be adjusted or removed. As long as the patient achieves spinal correction or reaches skeletal maturity with a curve less than 40 degrees, the VBT screws and cord remain in place.
“Patients are generally discharged from the hospital within one to two days following the procedure and often require minimal narcotic medication for pain management,” Dr. Serdahely says. “Most patients can resume their usual activities, including running, jumping, doing gymnastics and riding amusement park rides, approximately six weeks after VBT. In contrast, recovery after spinal fusion surgery is typically longer, resulting in a delayed return to school and sports.”
Advertisement
The ideal candidates for VBT are patients who have:
Patients usually are between ages 10 and 15. However, skeletal age (as determined by hand X-rays, using the Sanders staging system) is more important than chronological age.
Dr. Serdahely notes that spinal fusion may be preferable if a patient’s growth plates are closed or their spine curvature exceeds 65 degrees. VBT also is less suitable for younger patients with significant skeletal growth left, as there’s a risk of overcorrection.
“Still, VBT can be a good surgical option for select patients because it preserves motion and prevents the stress that fusion can place on spinal disks,” he explains. “That stress can lead to degenerative arthritis later in life.”
VBT preserves the option for spinal fusion later, if needed.
“Most pediatricians know that progressive scoliosis needs treatment, but many aren’t aware of VBT,” Dr. Serdahely says. “Spinal fusion isn’t the only option now. Motion-preserving growth modulation may help some children, so early referral while they’re still growing is essential.”
Advertisement
Advertisement

Early intervention yields the best outcomes, but surgery can benefit older patients as well

Cleveland Clinic pediatric spine surgeon shares his insights

Success for these complex operations requires judicious patient selection and presurgical patient optimization

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians