The art of refractive cataract surgery
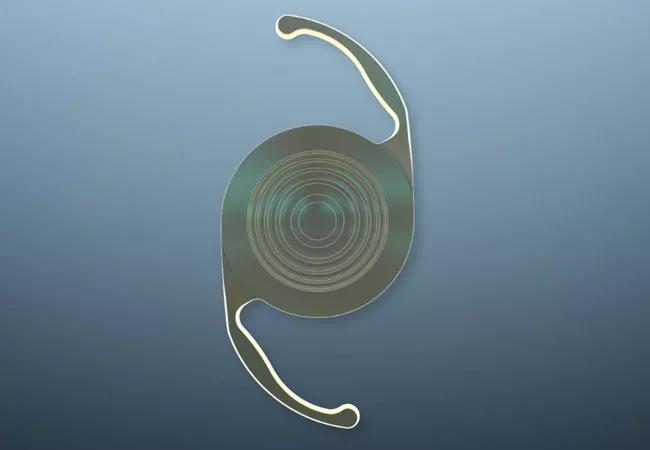
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e3dbcff7-ae3e-4b9d-b9a5-8b2be11a0079/20-EYE-1875113-IOLs-CQD-4_jpg)
20-EYE-1875113-IOLs-CQD-4
By Claudia Perez-Straziota, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The emergence of refractive cataract surgery has changed the approach to cataract surgery dramatically. Beyond visual rehabilitation, patients and surgeons both desire to minimize spectacle dependence after surgery, with reproducibly successful outcomes and satisfied patients.
There are multiple factors involved in refractive success, such as intraocular lens (IOL) power calculation and astigmatism management. However, two often overlooked issues are the management of higher order aberrations (HOAs) and the individualized approach to refractive lens selection.
For some time, HOAs have been recognized as critical factors in outcome of laser vision correction.1,2 Their specific role in cataract surgery, however, has been less appreciated until recently.
Most corneas are slightly prolate, with low levels of naturally occurring positive spherical aberration. Neutralizing this spherical aberration improves contrast sensitivity and best distance acuity but reduces depth of focus. Conversely, intentionally increasing spherical aberration can provide a wider range of focus.3 Thus, while in some patients the goal is to neutralize spherical aberration for optimal binocular distance acuity, in others inducing spherical aberration in the near targeted eye can improve visual performance at intermediate distance when targeting blended vision with monofocal IOLs.
In patients with prior laser vision correction, both IOL power calculations and HOA evaluation require additional focus. These patients expect to maintain the same spectacle independence that they enjoyed after refractive surgery. Therefore, because routine IOL formulas cannot accurately determine optimal lens power, adjustments must be made to improve accuracy and minimize refractive surprises.4 Additionally, these patients’ HOA profiles are frequently altered postoperatively and require special attention to avoid exacerbating spherical aberrations and maximize visual quality.5 Monofocal IOLs are available in both negative spherical platforms (which can compensate the positive spherical aberration resulting from myopic ablations) and positive spherical platforms (which can compensate the negative spherical aberrations induced in hyperopic ablations).
Advertisement
With the Food and Drug Administration’s recent approval of trifocal lens technology, we now have bifocal, trifocal and extended depth of focus lens technology available for our patients. With so many IOL choices, the preoperative evaluation process is critical and must extend beyond straightforward ophthalmic examination and basic biometry. Refractive IOLs are particularly sensitive to corneal irregularities, and proper selection of candidates for these IOL platforms is critical.6
Irregular astigmatism impacts visual quality, is often not easily manageable, and can be easily overlooked if a dedicated assessment and management plan of ocular surface and HOAs is not incorporated into the standard preoperative cataract evaluation. Patients with coexisting chronic ocular surface disease, most commonly non-Sjögren’s keratoconjunctivitis sicca, tend to have significant surface irregularity. The management of ocular surface prior to IOL calculation can prevent a surgeon from having a very dissatisfied patient.
Patients with more advanced disease, who have been unresponsive to different topical therapies and have continued fluctuations in corneal topography, are not good candidates for any multifocal IOLs, since these platforms will add distortion to the inherent multifocality in their cornea.
In addition to dry eye, other corneal irregularities can be treated prior to cataract surgery, turning some patients into good candidates for premium IOLs. A common example in our practice is patients who present for cataract evaluation with epithelial basement membrane dystrophy or Salzmann’s nodular degeneration. They can receive refractive IOLs after regularization and stabilization from superficial keratectomy.
Advertisement
Once a patient is deemed a good candidate for refractive IOL platforms, it is important to consider that each patient has different vision needs, and each will benefit from a different approach. For example:
Even though the latest trifocal IOL platforms provide the widest range of vision, an 80-year-old woman who likes to knit will not enjoy the compromise in near vision and may benefit more from the +3.00 add multifocal platform. The same 80-year-old woman who enjoys watching TV may, in contrast, enjoy the range of focus from trifocal IOLs.
Ultimately, the most satisfied patients are those who actively participate in developing their own surgical plan. Our role is to provide patients with an educated recommendation. During cataract evaluation visits at Cole Eye Institute, after a thorough evaluation (including a full eye exam and thorough assessment of the ocular surface and specific anatomical features that may or may not make the patient a good candidate for a refractive IOL) we dedicate time to educating patients about our findings and addressing their expectations and specific visual needs.
The art of IOL customization goes beyond the numbers. We must see our patients as individuals with different visual needs. Not all IOLs are good for all patients.
Advertisement
Dr. Perez-Straziota is a staff member of Cleveland Clinic’s Cole Eye Institute.
Feature image courtesy of Alcon.
Advertisement
Advertisement
A review of pathophysiology, risk factors, clinical presentation and treatment options
How computational tools and personalized biomechanics can improve keratoconus detection, ectasia risk assessment and surgical outcomes
Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma
Registry data highlight visual gains in patients with legal blindness
Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence
A look at emerging technology shaping retina surgery
A primer on MIGS methods and devices
7 keys to success for comprehensive ophthalmologists