Is disorganization of retinal inner layers (DRIL) a useful prognostic indicator?
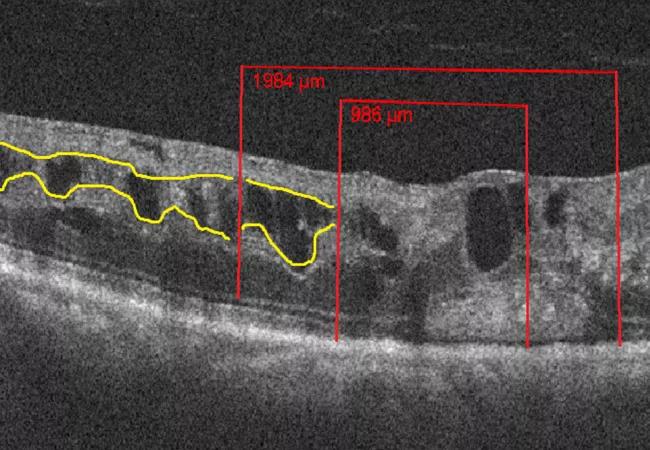
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6c2167c3-c46f-41ff-a064-925342c6ba5c/18-EYE-4207-DRIL-CQD-Feat-1_jpg)
18-EYE-4207-DRIL-CQD-Feat
By Amy S. Babiuch, MD; Michael Han, BS; Felipe F. Conti, MD; Karen Wai; Fabiana Q. Silva, MD; and Rishi P. Singh MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In previous studies, the disorganization of retinal inner layers (DRIL) has demonstrated its ability to help determine visual acuity (VA) prognosis in diabetic macular edema that requires treatment. Given this association, our Cole Eye Institute group studied how DRIL may affect VA outcomes in patients with retinal vein occlusion (RVO) undergoing treatment for secondary macular edema.
DRIL is defined as the extent to which there is a failure in the recognition of any of the demarcations between the ganglion cell-inner plexiform layer complex, inner nuclear layer, and outer plexiform layer on optical coherence tomography (OCT). This is demonstrated in Figure 1 where yellow lines course through the areas of normal demarcation and stop at those areas with poor demarcation.
We performed a retrospective study of 147 eyes from 147 patients with treatment naïve RVO and a minimum of 12 months follow-up. Seventy-five eyes had central retinal vein occlusion (CRVO) or hemi-retinal vein occlusion (HRVO), and 72 eyes had branch retinal vein occlusion (BRVO). Among the 147 patients, the mean patient age was 68.9 years, 75 (51 percent) were female and 72 (49 percent) were male. Baseline DRIL was identified in 61.9 percent of all eyes (91/147).
We used a presence or absence approach to score DRIL across three regions on the horizontal OCT line scan at baseline, six months, and 12 months. Figure 1 demonstrates how the horizontal line scan was broken down into regions. At six and 12 months, DRIL scores were further evaluated for stable, increasing or decreasing DRIL burden.
Advertisement
At six months, DRIL scores in all regions demonstrated a decrease in detection, however, at 12 months, all regions revealed a modest increase in DRIL detection (Figure 2).
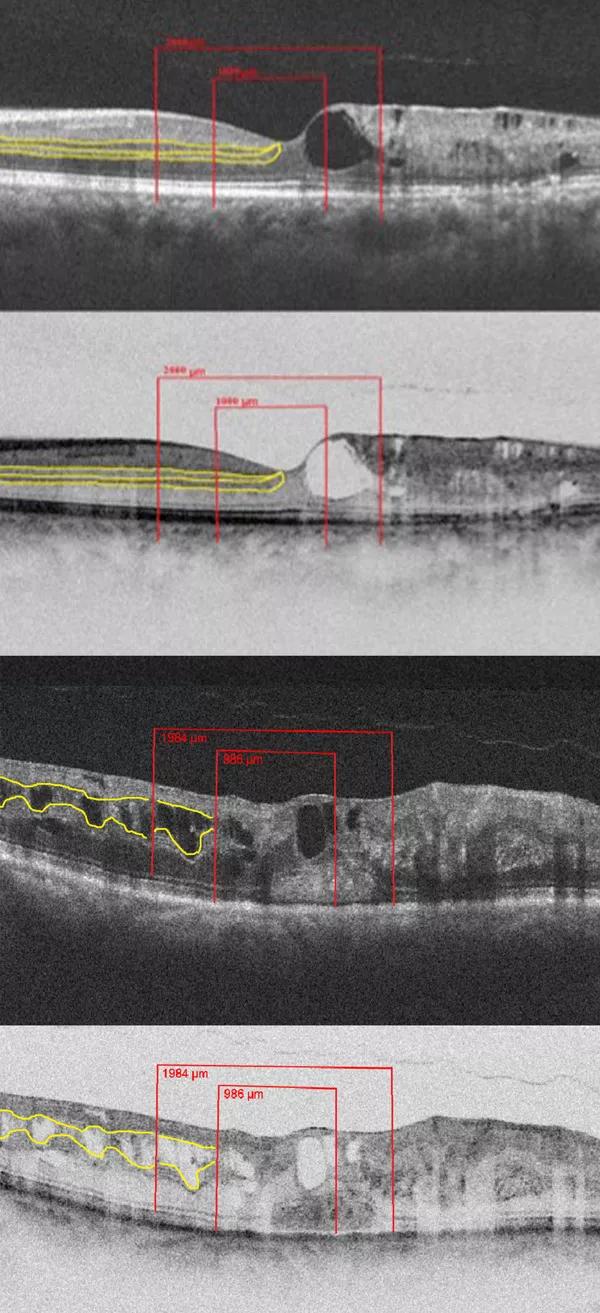
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e73d67a1-7743-4cb7-8254-7dad5cc03b64/18-EYE-4207-DRIL-CQD-F1_jpg)
Figure 1. Spectral domain OCT (SD-OCT) representing the regional division of the SD-OCT outlined by red lines, and the inner retinal interfaces highlighted by yellow lines that disappear in the areas of DRIL in two representative cases. The top two images are from a patient with a BRVO and the bottom two images are from a patient with a CRVO. Both cases exhibit intraretinal fluid and DRIL in all three regions on SD-OCT and on reverse gray-scale SD-OCT.
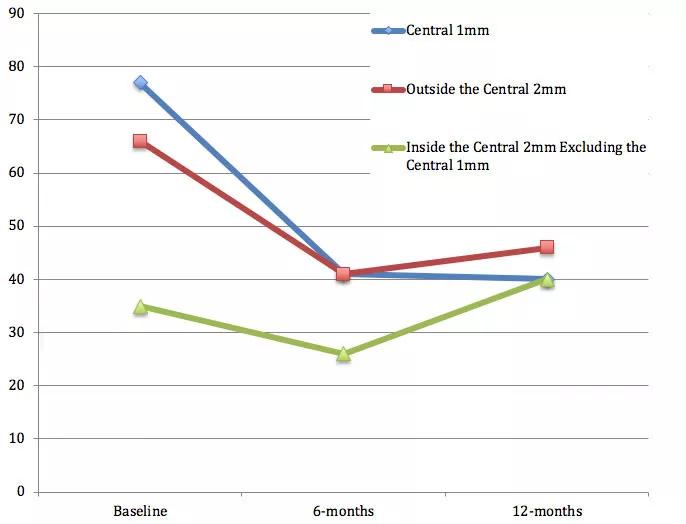
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f620160f-2857-45ae-8500-991630321a51/18-EYE-4207-DRIL-CQD-F2_1_jpg)
Figure 2. Changes in DRIL Over Time. At the six-month time point, all regions demonstrated a decrease in DRIL detection as compared to baseline. However, at 12 months, all regions revealed a modest increase in DRIL detection as compared to the six-month time point.
When we compared this to the number of anti-VEGF (vascular endothelial growth factor) injections delivered, we found that the average number of injections decreased by about half in months six to 12 as compared to the first six months in both groups (Figure 3). This decline in treatment with anti-VEGF agents may have allowed for progression of disease and worsening DRIL scores in months six to 12.
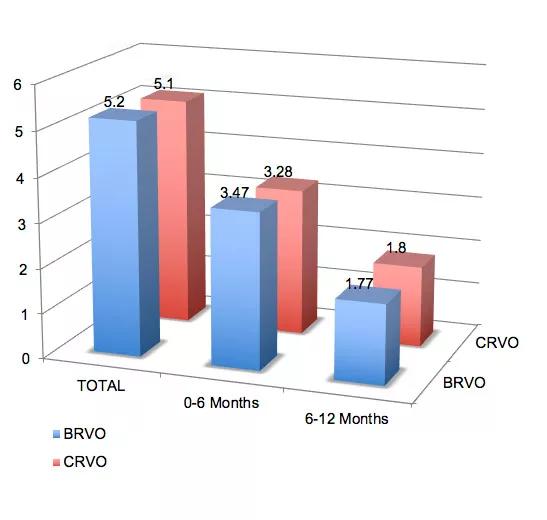
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1ccc6d5f-ec18-449f-8881-1d2c0791b7d3/18-EYE-4207-DRIL-CQD-F3_jpg)
Figure 3. Number of Anti-VEGF Injections Delivered Over Time. Total number of anti-VEGF injections was roughly equal between both the BRVO and the CRVO groups. The number of anti-VEGF injections delivered declined in the six- to 12-month time period as compared to the zero- to six-month time period in both groups.
Advertisement
Based on the results of our study, we concluded that the presence of DRIL at baseline in BRVO patients is associated with worse baseline VA. Increasing DRIL burden in CRVO and HRVO patients is associated with reduced VA gains.
Baseline DRIL presence and changes in DRIL burden during the course of disease in RVO is a useful prognostic indicator for VA and can help guide treatment with anti-VEGF therapy.
Mr. Han and Ms. Wai are medical students; and Drs. Conti and Silva were visiting research fellows. Dr. Babiuch presented this study on the podium at the 2018 American Society of Retina Specialists (ASRS) Annual Meeting, and it has been accepted for publishing in JAMA Ophthalmology.
Advertisement
Advertisement
A review of pathophysiology, risk factors, clinical presentation and treatment options
How computational tools and personalized biomechanics can improve keratoconus detection, ectasia risk assessment and surgical outcomes
Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma
Registry data highlight visual gains in patients with legal blindness
Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence
A look at emerging technology shaping retina surgery
A primer on MIGS methods and devices
7 keys to success for comprehensive ophthalmologists