Cleveland Clinic's Hearing Implant Program’s minimalist approach to osseointegrated implants emphasizes an easy patient experience.
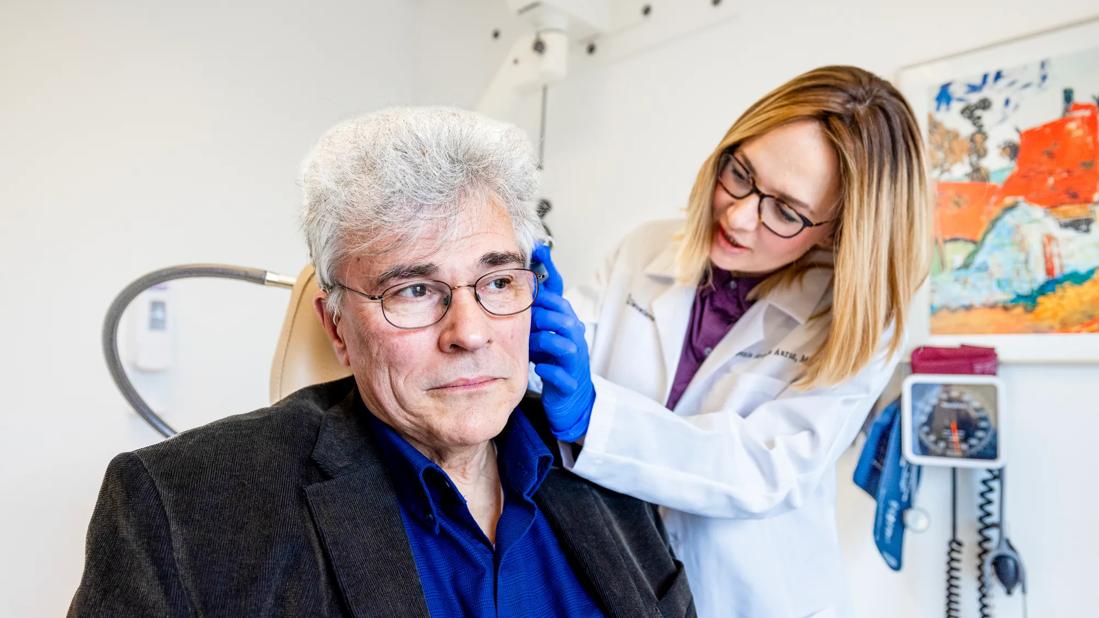
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/33c16a99-cec0-4639-a822-cae4d063808d/HNI_4608508_02-09-24_055_LDJ-jpg)
osseointegrated implant surgery
For patients with conductive or mixed hearing loss, auditory osseointegrated implant surgery can be life-changing. However, traditional implant surgery has been intimidating to patients. To overcome these barriers to patient acceptance, the Cleveland Clinic Hearing Implant Program (HIP)’s team of neurotologists and audiologists offer patients osseointegrated implants with a very streamlined surgery and recovery process. Their approach drastically decreases surgical time, with almost no down-time for the patient after surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Osseointegrated implants work by rerouting sound, which is distinctly different from a cochlear implant. While a cochlear implant helps restore hearing in an ear with sensorineural hearing loss, an osseointegrated implant is used to re-route sound to a functional cochlea. It is FDA approved for patients who have conductive or mixed hearing loss, or single-sided deafness (SSD) when the other ear hears normally.
Many individuals have conductive or mixed hearing loss related to prior ear surgery or infections. These patients make up the bulk of the CCF HIP team’s osseointegrated implant recipients. “A classic example is a patient who’s had a modified radical mastoidectomy,” says Erika Woodson, MD, the Section Head of Neurotology/Otology/Lateral Skullbase Surgery and the Medical Director of HIP. “They are likely missing ossicles, and do not have direct surgical options to restore hearing.” Additionally, their mastoid cavity is not a healthy hearing aid environment. “These ears may start to have chronic drainage or infection when they try to wear hearing aids directly in the ear,” remarks Dr. Woodson.
Another potential candidate is the patient with SSD. “If somebody has complete deafness on one ear and a normal ear on the other side, they can receive an osseointegrated implant on the deaf side that takes sound over to the good ear,” explains Anh Nguyen-Huynh, MD, Staff Neurotologist. “This requires that the inner ear works normally on the side receiving the sound. In this situation, we place the implant on the bad side. But, instead of trying to send sound into the bad ear, it sends sound around to the other side through bone conduction.”
Advertisement
Dr. Woodson notes that although CCF HIP surgeons and audiologists now routinely recommend cochlear implantation as a patient’s best option, several patients may not have that option. Insurance coverage for CI for SSD is still evolving, and patients’ plans may not yet extend coverage for the device. Additionally, some patients may not be a candidate for CI, for example, patients who lack an auditory nerve after vestibular schwannoma surgery, or pre-lingual congenital deafness beyond early childhood.
While osseointegrated implant technology has been around since the 1970s, the surgical methods have improved significantly. “The initial surgical technique involved extensive soft tissue removal, and the creation of a partial thickness skin graft to cover the area around the implant, which created a large wound to heal and an area of permanent hair loss,” explains Thomas Haberkamp, MD, Staff Neurotologist. This method was also performed under general anesthesia. Ten years ago, a popular method adapted a linear incision with more modest soft tissue reduction. This technique could be employed under general anesthesia or moderate sedation, and still required extensive healing time with the risk of alopecia around the abutment.
The surgical technique employed at Cleveland Clinic is the MIPS (Minimally Invasive Ponto Surgery) technique. Although multiple surgeons nationwide use this technique, Cleveland Clinic takes the “minimal” part even further.
“I think that’s one thing that really makes our program unique. We can offer the patient a very easy experience,” says Dr. Woodson. “Sure, we sometimes still use general anesthesia, but we can do the MIPS procedure on most adult patients under just light sedation. They don’t need full anesthesia; they don’t even need twilight anesthesia.”
Advertisement
Dr. Haberkamp explains that the scalp is numbed with an injection, and then a mild anxiolytic is administered while the surgery is performed. The whole procedure takes less than 10 minutes. The patient goes home with a dressing on their head; after removal the next day, there are no stitches and no visible wound to take care of, as a healing cap keeps the area hidden and clean. While they need to keep the area dry for the first week, they are able to continue their regular activities and they routinely return to work the next day. Most patients do not need narcotic pain control after surgery, Dr. Nguyen-Huynh notes.
When patients are considering options for this kind of surgery, offering them something that’s minimally invasive can be a major advantage, according to Dr. Woodson. “The difference between needing a mild sedative and needing a full anesthesia really impacts patients’ decision-making,” she says. “For patients who’ve been through perhaps multiple surgeries for chronic ear disease, they are resistant to undergo what feels like another major surgery. When I explain that it’s as simple as having dental work done, they’re far more receptive to exploring this option.”
In addition to minimizing a patient’s time commitment on the day of surgery, the HIP team also has taken care to streamline the patient’s postoperative experience as well. The surgeon team uses telemedicine to handle most patients’ postop visits. “We instruct them on how to properly take off their dressing in a five-minute face-to-face virtual visit,” says Dr. Woodson. “Many patients come from a distance for this procedure, so it’s wonderful that we can take them through the dressing removal and take a look at the implant from their own home.”
Advertisement
Cleveland Clinic’s HIP team allows the implant one month to heal before activation, the point at which the implant can be used with the external hearing processor. “The implant itself is just a metal post,” explains Dr. Haberkamp. “And the bone has to heal to that metal post—that’s why it’s called osseointegration.” After osseointegration has occurred, the audiologist sees the patient in-person to fit their external hearing processor to the implant. Most patients require very little ongoing follow-up with the audiologist after activation.
Manufacturers ensure their external processors are regularly updated with new technology, meaning the implant itself is never obsolete. “The implant itself has really changed very little since its original inception. The bulk of innovation occurs externally, by making these processors smaller, more energy-efficient, with improved sound quality and more power,” says Dr. Nguyen-Huynh. These newer processors are back-compatible with the patient’s implant, meaning that they’ll always be updatable without more surgery.
Patients with chronic ear disease and conductive/mixed hearing loss frequently fight with their hearing aids, going back and forth between infections/drainage and the periods of disuse these infections cause. For many of these recipients, an osseointegrated implant has made a tremendous difference to their aural toilet and frequency of infections. Additionally, the sound quality of these implants is typically night-and-day better than their old hearing aids, notes Dr. Haberkamp.
Advertisement
Dr. Woodson notes that her osseointegrated implant patients are generally some of her most content. “Almost universally, people love them,” Dr. Woodson enthuses. “So we sought to remove as much intimidation around getting the surgery as possible. It’s rewarding to give these patients an easy, yet life-changing, option for their hearing loss.”
At the Head & Neck Institute, the neurotologists performed 25 osseointegrated implant surgeries in 2019. In addition to the standard percutaneous abutment discussed here, the program offers several transcutaneous osseointegrated hearing implants as well as pediatric osseointegrated implant surgery.
Advertisement
Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor
Case study illustrates the potential of a dual-subspecialist approach
Evidence-based recommendations for balancing cancer control with quality of life
Study shows no negative impact for individuals with better contralateral ear performance
HNS device offers new solution for those struggling with CPAP
Patient with cerebral palsy undergoes life-saving tumor resection
Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition
Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.