Reconstruction using minimal access approaches

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/83da59e6-6929-40a1-bd1e-b8f8103351b4/17-ENT-4068-Fritz-Hero-Image_650x450pxl_jpg)
17-ENT-4068-Fritz-Hero-Image_650x450pxl
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Defects of the palate are standardly managed with locoregional flaps, effectively utilizing adjacent palatal, pharyngeal and buccal tissues for larger repairs. In the setting of larger defects or surgical sites compromised by scar, radiation or tissue ischemia, success with use of adjacent tissues becomes less likely and free tissue transfer techniques are the most viable surgical option. However, given the traditional morbidity and complexity of free flap reconstruction, management of many of these defects has been relegated to construction of palatal obturators.
While prosthetic reconstruction effectively manages the speech and eating impairments conferred by palatal defects, many patients are unsatisfied with the need for an appliance to restore normal function. Furthermore, the need for regular cleaning and irrigation of the defects to manage crusting and the potential for functional compromise if a prosthesis is lost or damaged are often sources of chronic patient concern.
Success rates and morbidity in microvascular reconstruction continue to increase and decrease, respectively. Minimal access approaches and improvements in harvest site techniques have played a significant role in decreasing operative times and hospital stays.1 Use of the anterolateral thigh flap in particular has led to a dramatic decrease in harvest site morbidity.2 As a result, in selected patients undergoing free tissue transfer, early discharge on postoperative days one through three has been employed without compromising outcomes or flap survival.3 All of these advances have allowed for expanded indications for free tissue transfer at Cleveland Clinic.
Advertisement
Surgeons in the Section of Facial Aesthetic and Reconstructive Surgery in the Head & Neck Institute have combined the above techniques and strategies to address defects of the hard palate reliably and with minimal morbidity. Indications for use of free tissue techniques include: 1) failed locoregional flap attempts with substantial residual fistulas, 2) previous or planned radiation therapy, 3) ischemic or blast mechanisms for fistula creation (e.g., cocaine, vasculitis, gunshot wounds) and 4) large areas needing reconstruction which are not amenable to locoregional flaps.
Defects involving minimal soft palate were managed with vascularized fascia lata perforator flaps. These flaps carry the advantages of minimal soft tissue bulk, ease of inset and rapid mucosalization.2 Vascular pedicles were tunneled from the oral cavity to minimal access incisions at the facial notch, nasolabial fold, or preauricular region where microvascular anastomoses were performed.
This technique has been performed in 14 patients with complete closure of the palatal defects in all patients. Twelve patients were started on oral diets on postoperative day one and all were on a soft diet by day two. All patients were ambulating at discharge and no patients experienced long term donor site morbidity. Average hospital stay after surgery was 2.8 days, with six patients discharged on postoperative day two or earlier. One patient experienced a postoperative donor site seroma and there were otherwise no perioperative or postoperative complications. Two patients required local flap revisions to successfully close small residual defects and no patients experienced long-term velopharyngeal insufficiency or dysphagia.
Advertisement
In conclusion, using ALT fascia lata perforator flaps and minimal access techniques, the morbidity of free flap reconstruction can be reduced substantially. This method allows for reliable repair of complex defects of the hard palate with shortened hospital stays and rapid return to full activity. As a result, the minimal access vascularized fascia lata flap appears to provide a more attractive alternative to traditional free tissue transfer or long-term obturator use.
Dr. Fritz is Section Head of Facial Plastic and Microvascular Surgery in Cleveland Clinic’s Head & Neck Institute.
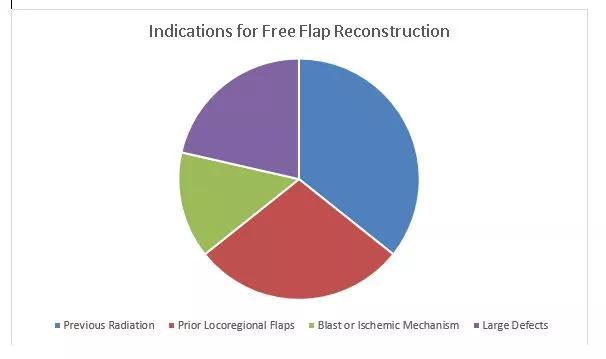
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/21939636-c45f-4b20-b7f1-1f4fbbb1a3b8/Capture_jpg)
References:
1 Knott PD, Seth R, Waters HH, Revenaugh PC, Alam D, Scharpf J, Meltzer NE, Fritz MA. Short-term Donor Site Morbidity: A comparison of the anterolateral thigh and radial Forearm fasciocutaneous free flaps. Head and Neck. 2016 Apr; 38(1):945-8
2 Revenaugh PC, Haffey TM, Seth R, Fritz MA. Anterolateral thigh adipofascial flap in mucosal reconstruction. JAMA Facial Plast Surg. 2014 Nov-Dec;16(6):395-9.
3 Revenaugh PC, Fritz MA, Haffey TM, Seth R, Markey J, Knott PD. Minimizing morbidity in microvascular surgery: small-caliber anastomotic vessels and minimal access approaches. JAMA Facial Plast Surg. 2015 Jan 1;17(1):44-8.
4 Devine CM, Haffey TM, Trosman S, Fritz MA. Short stay hospital admission after free tissue transfer for head and neck reconstruction. Laryngoscope 2016 Dec; 126 (12): 2679-2683
Advertisement
Advertisement
Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor
Case study illustrates the potential of a dual-subspecialist approach
Evidence-based recommendations for balancing cancer control with quality of life
Study shows no negative impact for individuals with better contralateral ear performance
HNS device offers new solution for those struggling with CPAP
Patient with cerebral palsy undergoes life-saving tumor resection
Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition
Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.