Retrospective study finds benefits of ultra-early therapy extend to this understudied subgroup
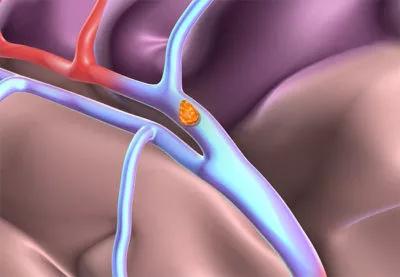
Early thrombolysis for acute ischemic stroke due to emergent large vessel occlusion (ELVO) is good, but ultra-early thrombolysis is even better. So suggests a retrospective study reported out of Cleveland Clinic’s Cerebrovascular Center and published in Journal of the Neurosciences.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Patients receiving intravenous tissue plasminogen activator (IV tPA) within 60 minutes of the onset of stroke symptoms (the “golden hour”) had significantly higher complete recanalization rates, better chance of early neurological improvement, and more favorable clinical outcomes and lower mortality at 90 days compared with patients treated beyond 60 minutes.
“Stroke due to ELVO has traditionally been thought to be less responsive to IV tPA compared with stroke due to non-large vessel occlusions,” says the study’s senior author, M. Shazam Hussain, MD, Director of Cleveland Clinic’s Cerebrovascular Center. “Other studies have evaluated outcomes after ultra-early administration of IV tPA for stroke of any cause, but data for the subgroup of ELVO strokes have been scarce. We hypothesized that giving IV tPA within the first 60 minutes since the patient was last known well — the so-called golden hour — increases rates of recanalization in ELVO and confers improved clinical outcomes.”
To test that hypothesis, he and colleagues identified all patients treated with IV tPA for acute ischemic stroke due to ELVO at Cleveland Clinic in the years 2013-2016. Of 201 patients identified, 158 had sufficient data for inclusion in the analysis. Among these patients, 25 (16%) received IV tPA within 60 minutes of their time last known to be well and 133 (84%) received IV tPA beyond 60 minutes. The two groups were comparable in terms of age, risk factors, baseline modified Rankin scale (mRS) score, initial NIH Stroke Scale score and distribution of arterial occlusion sites.
Advertisement
Compared with patients receiving IV tPA beyond 60 minutes, those receiving it within 60 minutes had favorable results on all key outcomes of interest, including:
“Because the amount of salvageable brain tissue diminishes quickly during ischemia, every minute counts when treating patients with acute ischemic stroke,” says Dr. Hussain. “This study demonstrates that this principle appears to apply in the context of ultra-early treatment of ELVO as well. This is important, as ELVO strokes account for up to half of ischemic strokes.”
He and his co-investigators write that these findings may be due to greater susceptibility to chemical thrombolysis when clots are freshly formed.
Dr. Hussain notes that this study was prompted by observations made among patients with ELVO treated on Cleveland Clinic’s mobile stroke treatment unit. He says its findings underscore the importance of promoting early recognition and management of all types of suspected ischemic stroke on all fronts, from public education on the signs and symptoms of stroke to refining stroke systems of care to ensure timely transport of patients to a stroke center best matched to their specific needs.
Advertisement
The study authors write that their findings may help explain why a recent post hoc analysis of pooled results from the SWIFT and STAR multicenter trials failed to show a significant benefit from giving IV tPA before intra-arterial therapy in patients with acute ischemic stroke due to ELVO. They note that this analysis did not report the time between stroke symptom onset and IV tPA administration.
In contrast, they add, their findings are aligned with a recent meta-analysis suggesting that IV tPA may obviate the need for intra-arterial therapy in some patients with ELVO. More broadly, the authors conclude that their findings “suggest that recanalization rates increase with ultra-early IV tPA administration, thus supporting the idea of IV tPA and intra-arterial therapy being complementary therapies.”
Advertisement
Advertisement

An expert talks through the benefits, limits and unresolved questions of an evolving technology

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood