But it is no substitute for clinical judgment
Flow measurement to assess graft patency should be routinely performed for multiarterial grafting and off-pump coronary bypass, as well as in other situations when doubts about the integrity of a graft arise. Likewise, the use of flow measurement findings to inform optimal intraoperative decision-making requires a good understanding of techniques for graft patency assessment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
These are leading takeaways from an invited expert opinion by two Cleveland Clinic cardiothoracic surgeons recently published in JTCVS Techniques summarizing common problems affecting bypass grafts, techniques used to verify graft function and tips for interpreting flow measurements.
“Suboptimal flow measurements warrant investigation into possible sources of flow compromise but should not trigger an automatic graft revision,” says Faisal Bakaeen, MD, co-author of the piece along with his colleague Rami Akhrass, MD. “Surgeon judgment remains a key component of determining how to react in such situations.”
Multiarterial grafting is becoming a favored approach in coronary artery bypass graft surgery (CABG), with evidence mounting that graft patency and clinical outcomes are improved over saphenous vein or single internal thoracic artery grafts. At Cleveland Clinic, Dr. Bakaeen notes, multiarterial grafting is the default procedure unless contraindicated; it is used in about 30% of all CABG operations and for most patients undergoing elective CABG.
This trend has triggered the need for real-time assessment of graft patency. Properties of arteries make routine flow verification especially important: arterial grafts are more susceptible to dissections and hematomas that may compromise flow. They also have a more dynamic nature, with flow influenced by multiple factors, such as spasm, hemodynamic parameters and severity of target vessel stenosis. In addition, manual injection to test distal anastomotic flow is not possible in an in situ arterial graft.
Advertisement
“Intraoperative validation of graft patency provides the opportunity to correct any technical issues before closing the patient’s chest,” Dr. Bakaeen adds. “Having this extra information is important for both safety and peace of mind.”
According to the expert opinion piece, off-pump CABG — which is physiologically less invasive than traditional CABG and can benefit selected high-risk patients — also merits routine intraoperative flow assessment.
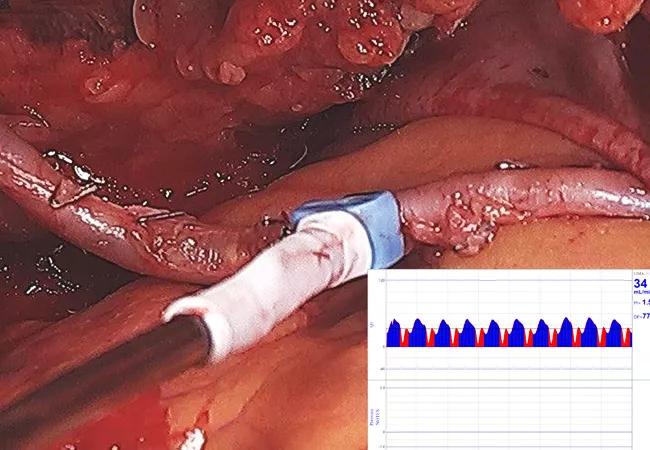
Methods of intraoperative graft patency assessment are described in the article. Coronary angiography, although often considered the gold standard for flow assessment, is impractical and not available in most operating rooms. Use of a transit time ultrasonic flow meter is covered in some detail, as is interpretation of its results. Epicardial ultrasonography, which is typically performed in conjunction with transit time flow measurement, is also discussed.
The authors note that flow assessment can be particularly useful in identifying a number of flow-limiting scenarios, including the following:
Advertisement
The article, which includes a short embedded video, summarizes leading observations and recommendations from the Cleveland Clinic experience. Dr. Bakaeen emphasizes the following messages:
“Flow measurements are an important supplement to a surgeon’s clinical judgment, and it is critical that he or she know how to employ and interpret them,” Dr. Bakaeen emphasizes. “Judgment remains the key component in determining how to react to a poor graft flow measurement, and it is what ultimately determines whether intraoperative flow assessment proves to be a friend or foe.”
Advertisement
Image at top: Photo showing assessment of an ITA graft with a transit time flow meter. Inset shows a resulting transit time flow measurement. Images are from Akhrass and Bakaeen. JCTVS Tech. 2021 Jan 5 [Epub]. © The Authors.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more