Cleveland Clinic report shares details and outcomes of novel technique for open repair

Superior vena cava (SVC) syndrome remains a challenging clinical entity, often leaving patients with debilitating symptoms even after aggressive endovascular management. A recent retrospective study from Cleveland Clinic, spanning more than two decades, suggests that autologous femoral vein is a viable and advantageous conduit for open surgical reconstruction of the SVC obstruction.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study (Vascular. 2025 Epub 15 Jan), which examined 10 patients undergoing central venous bypass or reconstruction using the femoral vein, demonstrated a primary patency rate of 79% at one year. Notably, every patient in the cohort experienced symptomatic relief following the procedure.
“In view of the recognized difficulty and potential for high recurrence rates associated with endovascular options, particularly in complex or recurrent benign obstructions, this operation offers an effective opportunity for long-term relief in severely impacted patients,” says senior author Sean Lyden, MD, Chair of Vascular Surgery at Cleveland Clinic. “Our findings suggest that the femoral vein should be strongly considered as the conduit of choice for open repair, as it offers potential benefits in procedural efficiency and size matching compared with the traditionally favored spiral great saphenous vein (SGSV) graft.”
SVC syndrome is characterized by venous congestion in the head and neck, often presenting as swelling in the face, neck and upper extremities. While it traditionally has been caused by external compression from mediastinal masses or tumor infiltration, recent decades have seen an increase in SVC syndrome caused by iatrogenic factors, specifically intracardiac pacemakers and indwelling central venous catheters (CVCs). In fact, the etiology in this study’s cohort was entirely iatrogenic, split evenly between pacemaker-related disease (n = 5) and CVC-related disease (n = 5).
Advertisement
Initial management frequently involves endovascular techniques aimed at regaining luminal expansion. While successful in select patients, endovascular treatment does not resolve symptoms in others and may be followed by lesion recurrence requiring reintervention. For patients with refractory symptoms or complex lesions that are better suited for open repair, surgical reconstruction is required.
Traditionally, surgical reconstruction has involved use of the SGSV graft, which has yielded some of the best published outcomes. However, creation of the SGSV graft is surgically complex and demands a substantial portion of saphenous vein to achieve adequate conduit length. In view of these challenges, the Cleveland Clinic team sought to review their institutional experience using the femoral vein — a conduit they have successfully used in infected aortic and peripheral reconstructions — for SVC repair.
The authors searched for all patients who underwent open SVC reconstruction or innominate vein bypass using the femoral vein at Cleveland Clinic from 2000 through 2023. Ten consecutive patients (five men, five women) were identified, with a mean age of 51.88 (± 10.20) years).
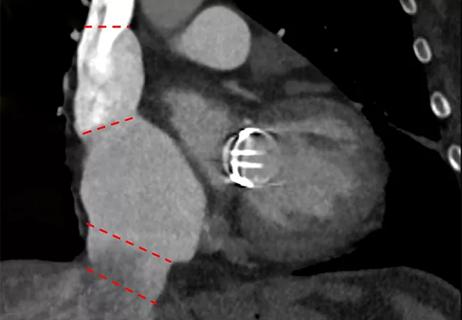
The severity and location of the SVC disease were assessed using venography and/or CT venogram. Seven of the 10 patients had undergone endovascular interventions (all at outside hospitals with limited records available) before referral for open surgical repair. Among those seven, four had experienced failed stents. Presenting symptoms included head or neck fullness (n = 5) and upper extremity swelling (n = 4).
Advertisement
Before harvest, bilateral femoral veins were assessed using duplex ultrasound to ensure patency and adequate vein size. Veins larger than 7 mm in diameter were deemed adequate for use. The femoral vein was harvested unilaterally from the adductor hiatus to the largest profunda branch.
In their study report, the authors outline a key technical detail of their procedure relating to size-based considerations in conduit preparation. Veins with diameters exceeding 10 mm were typically inverted before use. For smaller veins (< 10 mm), the technique of paneling was employed. Paneling involves harvesting twice the length needed, incising the vein longitudinally, excising the valves and folding the vein to half its original length. By sewing the long sides together and cutting the folded edge, the resulting new lumen has roughly twice the diameter of the original vein.
“This technique of modifying the vein to double the conduit diameter is simpler than spiral vein grafts in terms of preparation and planning,” Dr. Lyden explains.
Following the procedure, all patients were placed on anticoagulation therapy and prescribed lower extremity compression to promote patency and mitigate potential harvest-related complications. The patients’ average length of stay was 11 days (range, 6 to 26).
The cohort’s median follow-up period was 21 months (range, 3 to 48). The main efficacy findings supported use of the femoral vein as an acceptable conduit:
Advertisement
No mortality was observed. One patient developed tamponade physiology secondary to a pericardial effusion, managed successfully with a drain. Another patient was conservatively managed for a pneumothorax upon perioperative readmission.
Of note, graft surveillance revealed restenosis in two patients at the right atrial junction anastomosis. Both cases were managed endovascularly, first with drug-coated balloon angioplasty, with one requiring subsequent covered stent placement.
The meticulous harvest techniques and mandated use of lower extremity compression appeared effective in preventing common harvest-related adverse events. Serious complications noted in other series — such as deep venous thrombosis, compartment syndrome, or chronic venous insufficiency in the harvested limb — were not observed.
“The outcomes in this series indicated that femoral vein reconstruction is a promising approach that offers acceptable venous patency rates and good symptom relief for SVC obstruction,” Dr. Lyden says. “The ability of the femoral vein to provide adequate size matching for SVC reconstruction is a significant advantage. And the paneling technique provides an efficient way to increase the vein’s caliber when needed.”
The authors note that while 79% primary patency at one year is encouraging and at least as good as the patency reported in some prior studies of various conduits, including spiral vein grafts, they acknowledge the limitations of their small, single-center, retrospective series. They call for larger, prospective trials and comparative studies to validate these findings and firmly establish the long-term effectiveness of femoral vein reconstruction relative to endovascular stenting or alternative surgical approaches.
Advertisement
“Pending further data from such trials, this experience supports the femoral vein as a favored conduit at our institution for treating severe, refractory SVC syndrome, Dr. Lyden observes.
“In our experience, the deep femoral vein provides the ideal combination of caliber, wall strength and long-term durability for SVC reconstruction,” adds cardiothoracic surgeon Edward Soltesz, MD, MPH, who wasn’t involved in the study. “We’ve seen far superior patency and symptom relief compared with other autologous or prosthetic options, making this our preferred conduit in collaboration with vascular surgery for complex SVC syndrome repairs. Anyone suffering from SVC syndrome should be evaluated to see if this operation is right for them. Recovery is typically rapid, and the relief of symptoms can be truly life-changing.”
Advertisement

Novel approach outperforms standard of care for post-PVI stenosis and occlusion
Understanding VC anatomy is critical for transcatheter tricuspid valve interventions

Scenarios where experience-based management nuance can matter most

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center