Either repair or replacement of native valve can yield low mortality, excellent results
Whether valve repair for isolated native mitral valve (MV) endocarditis is better than valve replacement depends on patient characteristics and pathology, with no difference in outcomes between the two approaches in the setting of extensive valve destruction. Moreover, dialysis and renal failure are the most important determinants of outcomes, not type of surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
These findings emerged from an extensive review of Cleveland Clinic experience over nearly two decades, in what may be the largest series to examine patient, microbiological, pathological and procedural factors related to outcomes of surgery for isolated MV endocarditis. The retrospective study was recently published in the Journal of Thoracic and Cardiovascular Surgery.
“We found that the traditionally regarded superiority of mitral valve repair is actually related to patient and pathological factors, as healthier patients tend to be selected for standard repair,” says the study’s corresponding author, Eugene Blackstone, MD, Head of Clinical Investigations in Cleveland Clinic’s Miller Family Heart, Vascular & Thoracic Institute. “Whether to replace or repair a native valve should be determined by valve pathology, a surgeon’s ability and experience, and patient factors such as surgical risk and life expectancy.”
Most studies have concluded that native valve repair leads to better outcomes over replacement in patients with isolated MV endocarditis, leading to fewer reinfections and reoperations. However, standard repair techniques are insufficient when there is extensive pathology, and individual patient characteristics may also favor replacement over repair. For patients with prosthetic MV endocarditis, replacement is the only surgical option.
The current study was conducted to investigate valve features and clinical factors of patients who underwent either repair or replacement for isolated MV endocarditis and these variables’ associations with outcomes.
Advertisement
Between January 2002 and January 2020, 447 operations were performed for isolated MV infective endocarditis at Cleveland Clinic in 429 unique patients. Of these, 326 patients had native valve endocarditis, of whom 88 (27%) underwent standard MV repair, 43 (13%) underwent extended repair (two cases after previous repair) and 195 (60%) underwent valve replacement. All patients with a prosthetic valve (n = 103) underwent valve replacement.
Among patients with native valve endocarditis, 282 had untouched valves and 44 had a previous valve repair, with the latter group presenting with more cardiac morbidity.
For risk-adjusted comparison, 70 variables were analyzed using random forest machine learning. The data — which included patient characteristics, operative and pathology findings, procedure details, microbiology results, echocardiography measures and hospital outcomes — were extracted from prospective quality registries. Patients had a median of 4.4 years follow-up.
Findings included the following:
Advertisement
“The decision to repair or replace did not turn out to be as important as we predicted,” says study co-author Shinya Unai, MD, a surgeon in Cleveland Clinic’s Department of Thoracic and Cardiovascular Surgery. “As baseline characteristics were the primary driver of outcomes, we carefully decide between extended repair versus replacement for the treatment strategy based on the intraoperative findings and patient background.”
In their study report, the authors highlight several takeaways from this investigation:
Advertisement
“The finding that valve management turned out not to be a risk factor for outcomes does not indicate that that the choice is irrelevant,” Dr. Blackstone emphasizes. “Instead, it suggests that surgeon judgment is critical for determining the appropriate approach.”
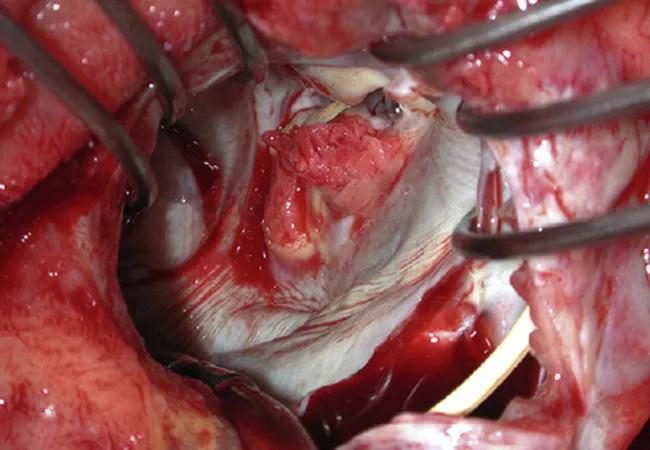
The image of mitral valve endocarditis at top is reprinted from Pettersson et al., “Infective endocarditis: An atlas of disease progression for describing, staging, coding, and understanding the pathology,” Journal of Thoracic and Cardiovascular Surgery. 2014;147:1142-1149. Copyright 2014, with permission from The American Association for Thoracic Surgery.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more