Procedure requires precision, has benefits for kidney donors

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2f0cd0cd-6cdc-44e2-8e57-b3ef6ee516f6/15-URL-063-Nephrectomy-690x380_jpg)
15-URL-063-Nephrectomy-690×380
By Shih-Chieh Jeff Chueh, MD, PhD, and Bashir R. Sankari, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Laparoscopic live-donor nephrectomy (LLDN) is the current surgery of choice for living kidney donors. According to a recent meta-analysis, laparoendoscopic single-site LDN (LESS-LDN) produces less pain, shorter recovery time and better cosmesis than does LLDN. However, LESS-LDN is extremely demanding on surgeons, due to its technical challenges and need for precision.
Here, we share our experience with LESS-LDN and describe our procedure. We also provide guidance on how to handle difficulties that could possibly emerge, and how to convert stepwise, if needed, to conventional laparoscopic LDN or open surgery for safe execution of this yardstick surgery.
With the donor in a 45° flank position and the donor kidney side up, a GelPort device was installed as the LESS platform at a 5 cm periumbilical midline incision. A large adhesive drape was applied over the abdomen, covering the whole GelPort (Figure 1). Through the gel-cap of the GelPort, 3 or 4 laparoscopic trocars were spaced apart to achieve triangulation and to avoid clashing of the instruments during LESS-LDN (Figure 1).
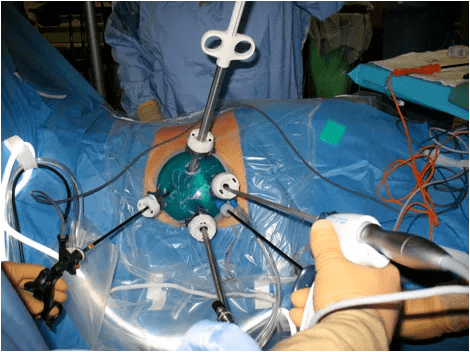
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ca35c1a6-d35d-4f61-8aa4-35859ab788ee/15-URL-063-Nephrectomy-fig1_png)
Figure 1.. External view of the ports and instruments during a laparoendoscopic single-site living donor nephrectomy.
Standard dissection of the kidney for donation with both curved and straight laparoscopic grasper and dissector was performed by ensuring that the kidney was well-perfused and the renal vein was nicely distended (Figure 2).
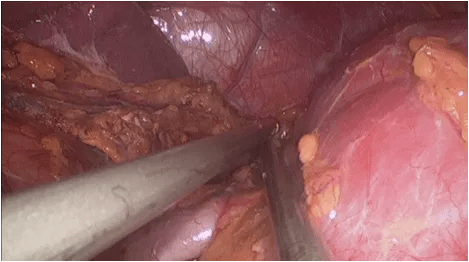
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/efc31027-10e5-4449-a2c2-9778c0d75b37/15-URL-063-Nephrectomy-fig2_png)
Figure 2. Laparoscopic view during a laparoendoscopic single-site living donor nephrectomy. Note the pink left kidney (to the right of the black instrument), and the well-distended left renal vein (between the two instruments).
Advertisement
Before renal hilar vessels were ligated separately with Endo TA™ staplers, a laparoscopic retrieving bag was inserted through the gel-cap to bag the kidney for tenting up the vessels, so that a longer pedicle could be harvested and to shorten the warm ischemic time. The kidney was removed through the LESS incision immediately after hilar vascular transection.
Using this technique, LESS-LDN was successful in all living donors without any multisite laparoscopic or open conversion, and without any instrument through extra wounds — although we would have done so if at any point we felt that this would have provided additional patient safety or facilitated the operation.
No patient experienced perioperative complications or received transfusions. Median operative time was 271 minutes, with a warm ischemia time of 3.5 minutes. Hospital stay averaged two days, with an average visual analog pain score of 4 of 10 at discharge and 2 of 10 at two weeks. All recipients had immediate graft function.
In case of difficulties, an extra one to two trocars can be inserted outside the LESS platform to achieve triangulation alignment with the umbilical incision. This immediately converts the surgery into a standard pure or hand-assisted LLDN. If the condition requires open conversion, upward extension of the midline incision to the subxyphoid area and rotation of the operating table will rapidly convert the procedure to an open surgery.
Using the GelPort as the access platform, LESS-LDN is feasible and safe. It can be easily converted to conventional laparoscopic LDN or open surgery, if necessary, to maintain the extremely high safety standard of LDN. This is especially attractive for less experienced surgeons.
Advertisement
Dr. Chueh is a staff member of Cleveland Clinic Glickman Urological & Kidney Institute’s Department of Urology and a Clinical Professor of Surgery at Cleveland Clinic Lerner College of Medicine. Dr. Sankari is Chief of the Surgical Subspecialties Institute at Cleveland Clinic Abu Dhabi.
Advertisement
Advertisement
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
Oncologic and functional outcomes are promising, but selection is key