NIH-funded comparative trial will complete enrollment soon
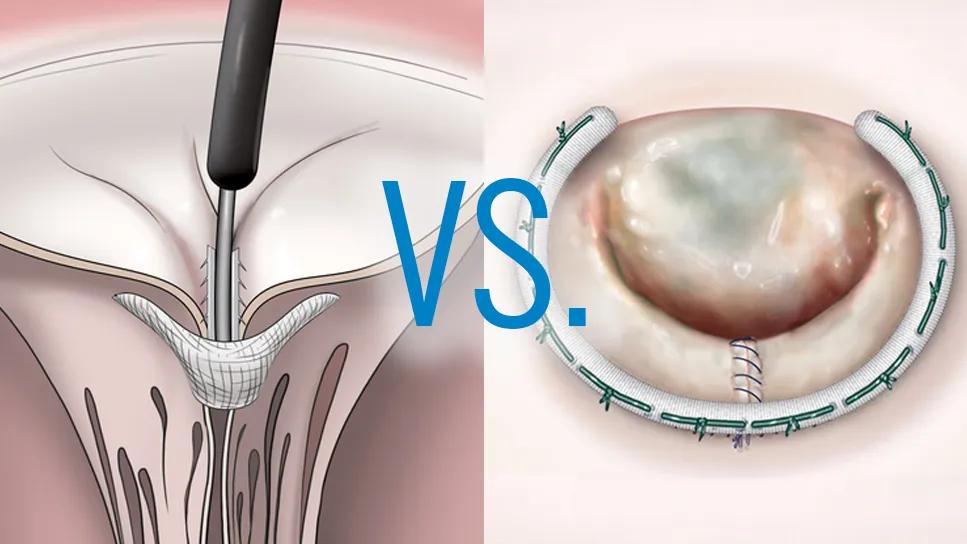
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c7287f3a-438d-49b4-86c6-36a82bb10c3b/MitraClipvsValve3)
illustrations of two valve procedures with "Vs." overlay spanning them
Transcatheter edge-to-edge repair of the mitral valve (M-TEER) has been approved in the U.S. for well over a decade, but robust data comparing M-TEER with surgical mitral valve repair have been relatively scarce. That will soon change thanks to the multicenter PRIMARY trial (NCT05051033), a leading study of the National Institutes of Health-funded Cardiothoracic Surgical Trials Network (CTSN). Enrollment will be completed by spring 2026, and first results are expected in late 2027 or early 2028.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Use of M-TEER has grown tremendously with limited data, and no previous trial has looked at longer-term results across the spectrum of patient risk,” says Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic as well as Chair of the CTSN and a PRIMARY trial investigator. “The PRIMARY trial is designed to determine which patients with primary degenerative mitral regurgitation [MR] are best served by surgery and which are best served by M-TEER.”
“This study is timely and relevant because use of M-TEER has grown despite the fact that the current FDA indication and American College of Cardiology guidelines endorse M-TEER only for patients at prohibitive risk from cardiac surgery,” says Amar Krishnaswamy, MD, Section Head of Invasive and Interventional Cardiology at Cleveland Clinic and a PRIMARY trial investigator. “Those recommendations are based on data published more than 13 years ago. Since then, numerous M-TEER device iterations have been made, imaging has advanced vastly for both MR diagnosis and procedural guidance, and patient selection has been refined. International registry data indicate that M-TEER results have improved substantially over that period, so we need a better understanding of how contemporary M-TEER compares with surgical mitral valve repair. PRIMARY is expected to provide that.”
PRIMARY is a prospective, open-label investigation among 450 patients aged 60 years or older with moderate to severe (grade 3+) or severe (grade 4+) primary degenerative MR. Participants are being randomized 1:1 to surgical mitral valve repair (with or without robotic assistance) or M-TEER with a commercially approved device at centers in the U.S., Canada and Europe (including Cleveland Clinic). Enrollees must be appropriate candidates for either surgical or percutaneous mitral valve repair and may be at any level of surgical risk — low, intermediate or high.
Advertisement
“This is the first trial of M-TEER to include low-risk patients,” notes Dr. Gillinov, who was involved in the study’s design and launch. “Notably, enrollees in PRIMARY have turned out to be mostly low-risk patients.”
“The current FDA indication for M-TEER translates mainly to use in patients who are quite elderly — around age 80 or even substantially older,” Dr. Krishnaswamy adds. “With transcatheter aortic valve replacement, we’ve seen patients who are much younger and in lower surgical risk categories achieve efficacy similar to what they’d get from surgery, but with less invasiveness. PRIMARY will help us formally assess whether that same principle applies to transcatheter treatment for the mitral valve, in terms of value for younger and lower-risk patients.”
The study’s primary endpoint is a composite of all-cause mortality, valve reintervention, hospitalization for heart failure or onset of ≥ 2+ MR (as measured by transthoracic echocardiogram) at three years after randomization.
Dr. Gillinov notes that the degree of MR in the composite endpoint was changed from an initial grade of ≥ 3+ at study launch. “We decided to ultimately require a surgery-like result, meaning mild MR or less, for any procedure in the trial to be considered successful,” he says. “We made the change because it’s increasingly recognized that residual regurgitation of moderate or greater severity is associated with shorter survival.”
Secondary outcomes include adequacy of MR correction, defined as < 2+ MR, at one year after randomization as well as quality-of-life measures. Outcomes will continue to be assessed over five years after intervention and out to 10 years for valve reintervention, quality of life and certain other endpoints.
Advertisement
The investigation is using a superiority design to detect any actual difference between the treatments rather than merely establishing noninferiority.
The superiority design is one of several distinctions between PRIMARY and another randomized trial comparing M-TEER and surgical mitral valve repair, the MitraClip REPAIR MR Study (NCT04198870), which is using a noninferiority design. That trial, sponsored by Abbott Medical Devices, recently completed enrollment.
REPAIR MR may prove less illuminating than PRIMARY because it is allowing moderate residual MR to be part of a successful outcome and is limited to patients at intermediate surgical risk. “I think the fact that PRIMARY is enrolling younger and lower-risk patients than REPAIR MR will provide better insights for real-world use of M-TEER,” Dr. Krishnaswamy says.
As enrollment in PRIMARY approaches completion, it is taking place against a backdrop of hypotheses that M-TEER’s reduced invasiveness and faster recovery may offer quality-of-life benefits while surgery may offer benefits in terms of repair durability.
The latter hypothesis received some support from a recent retrospective Cleveland Clinic study of midterm outcomes among 1,046 adults who underwent successful mitral valve repair with either transcatheter (n = 97) or surgical (n = 949) methods from 2014 through 2022 (Ann Thorac Surg. 2025 Epub 21 Aug). All patients had MR due to posterior leaflet prolapse. After propensity matching to identify 56 well-matched patient pairs, the study found that the M-TEER group developed more frequent and severe MR in the three years after intervention. “This suggests that surgery gave a more durable result, at least for this particular anatomy,” Dr. Gillinov notes, “although the study has the limitations of a retrospective analysis.”
Advertisement
It’s unlikely that PRIMARY will indicate that one therapy will be best for all patients, Dr. Gillinov adds. “We’re not looking for one therapy to ‘win’ but for the patient to win through clearer guidance on who should get which therapy,” he says.
Dr. Krishnaswamy concurs. “PRIMARY is a large trial that will yield a lot of granular data that should allow us to answer questions about particular anatomic subsets, such as specific areas where the valve has degenerated and how that might affect outcomes of surgery versus M-TEER,” he says. “All of that should help us understand which patients are better suited to one treatment or the other.”
He continues: “If the trial shows that M-TEER is a good alternative for surgical repair in some cases, it will still be imperative that M-TEER operators be selective and ensure that the anatomy they’re treating will be suitable for an M-TEER device.”
That argues for centers of excellence for both M-TEER and surgical mitral valve repair, which are in short supply. “Right now, which mitral valve treatment a patient gets depends in part on where they live and which doctor they see first,” Dr. Gillinov says. “In some parts of the country, they’re more likely to get M-TEER, whereas in others they’re more likely to get surgery. The goal of this study is to provide evidence to change that and guide physicians to provide the best therapy for a given patient.”
Advertisement
Advertisement
Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic
Why and how Cleveland Clinic achieves repair in 99% of patients
Two surgeons share insights on weighing considerations across the lifespan
An overview of growth in robot-assisted surgery, impressive re-repair success rates and more
Judicious application yields a 99.7% repair rate and 0.04% mortality
Cleveland Clinic series supports re-repair as a favored option regardless of failure timing
A call for surgical guidelines to adopt sex-specific thresholds of LV size and function
Cleveland Clinic series shows re-repair is feasible with excellent midterm results