Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic
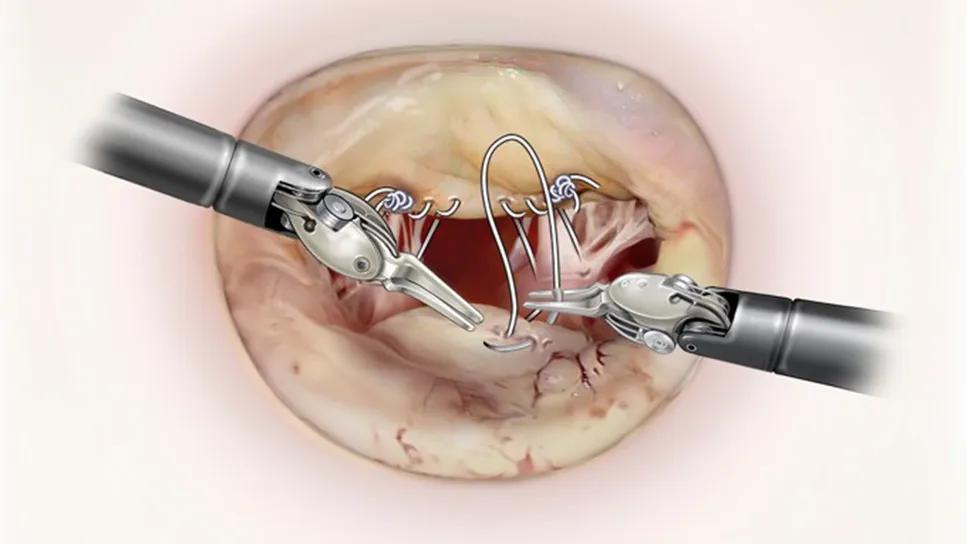
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9481fe71-e8ae-48f8-a0d1-213e7ebef6bf/robotic-MV-repair-feature)
illustration of two robot arms suturing a heart valve
Robotically assisted mitral valve repair differs from most other minimally invasive heart procedures in at least one key way, according to cardiothoracic surgeon Per Wierup, MD, PhD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Other minimally invasive treatments, whether surgical or catheter-based, tend to compromise visualization,” says Dr. Wierup, who was Europe’s premier mitral valve surgeon prior to joining the staff of Cleveland Clinic. “With robotic mitral valve surgery, the opposite is true: The magnification is so good and the 360-degree orientation is so revealing that it feels like I’m sitting inside the heart and seeing the mitral valve from there. As a result of this exceptional visualization, I believe I can do a better repair with the robot than without it.”
Beyond those benefits to the operator, robotic mitral valve repair confers numerous benefits to patients. In addition to the cosmetic advantages of much smaller incisions, patient benefits that have been documented in the literature include:
Such benefits for patient and operator alike have spurred increased use of robotic mitral valve surgery, with about 15% of mitral valve repairs in the U.S. in 2021 having been performed robotically (Ann Thorac Surg. 2024;117:96-104).
At Cleveland Clinic, use of the robot is considerably higher, with robot-assisted repairs now representing 70% to 80% of isolated mitral valve repairs performed at its Main Campus, up from 60% just a few years before.
“We’ve performed over 2,600 robotically assisted mitral valve operations to date, which is among the most of any center in the world,” says Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic and a mitral valve specialist. “What’s most important is that robotically assisted repair at our center is effective and safe, offering the same 99% rate of repair [versus valve replacement] and the same mortality of less than one death in 1,000 cases that we achieve with open repair.”
Advertisement
Those results prompted Cleveland Clinic’s Heart, Vascular and Thoracic Institute to acquire a second robotic surgery system in autumn 2025 — the new da Vinci 5™ platform. “This is the latest iteration of the robot,” Dr. Gillinov notes. “Unlike any other robotic system available, it has haptic feedback, offering tactile information to give operators the sense they are feeling tissue or feeling a suture. In contrast, every prior version has required surgeons to rely solely on what they can see with their eyes. With this addition, our Main Campus is one of the only places in the world with two dedicated cardiac robots.”
Cleveland Clinic’s use of the robot for a growing share of mitral valve repairs stems from the experience gained over 2,600+ robot-assisted repairs. “We are now fast with the robot, and we can tackle more complicated valves,” Dr. Gillinov explains. “We have developed alternate ways, if necessary, of hooking up the patient to the heart-lung machine and a better understanding of how to protect the heart during a robotic procedure.”
These insights are outlined in a new open-access article by Drs. Gillinov, Wierup and colleagues outlining their approach to patient selection for robotic mitral valve surgery (Curr Opin Cardiol. 2025 Epub 25 Aug). The paper captures the essentials of an algorithm the team developed to determine candidacy for a robotic approach, including how Cleveland Clinic uses preoperative coronary artery imaging, transthoracic echocardiography, and CT of the chest, abdomen and pelvis in this setting.
Advertisement
The paper reflects recent experience-based expansions of the algorithm to include consideration in patients with relative contraindications to a robotic approach — and the mitigation strategies to make robotic repair safe in these situations. Examples include:
“We consider all mitral valve repair patients to be potential candidates for robotic repair,” Dr. Wierup says. “Contraindications tend to involve factors outside of the mitral valve itself or the need for concomitant operations that cannot be performed robotically. Because of our experience, complexity of the mitral valve itself is not an obstacle to robotic repair for our team. For instance, we can robotically repair many valves with substantial mitral annular calcification using Gore-Tex techniques to create artificial chords. Another example is Barlow’s valve, which few centers will repair robotically. We have developed a technique using the robot where we use artificial chords to achieve a great repair of even severe Barlow’s valve in less than an hour of cross-clamp time” (see Figure).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b71350b5-0e05-4c2e-9808-961a35ec128d/robotic-MV-repair-inset)
Figure. Cleveland Clinic’s approach to robotically assisted repair of Barlow’s valve. (A) A typical Barlow’s valve with redundant leaflet tissue and bileaflet prolapse. (B) Robotic repair starts with creation of new chords to the anterior leaflet using PTFE sutures. (C) This is followed by creation of new chords to the posterior leaflet using the same technique. (D) The bileaflet prolapse is then treated. (E) The final step is correction of annular dilatation with a large, flexible annuloplasty.
The Cleveland Clinic algorithm has also been expanded to include patients who need other concomitant operations, including tricuspid valve repair with annuloplasty (often to address tricuspid regurgitation secondary to mitral regurgitation), surgical ablation of atrial fibrillation and closure of an atrial septal defect or patent foramen ovale.
Advertisement
“Cleveland Clinic is one of few centers with the expertise to do these concomitant procedures safely with the robot,” Dr. Gillinov notes. “In this context, safely means expeditiously, so that we don’t prolong the patient’s time on the heart-lung machine. That expeditiousness comes with frequent and regular use of the robot.” He adds that as Cleveland Clinic’s experience with robot-assisted aortic valve replacement and coronary artery bypass grows, those procedures might ultimately be considered in combination with robot-assisted mitral valve repair.
Now that robot-assisted mitral valve repair has such a well-established safety and efficacy record at experienced centers, interest in its impact on health-related quality of life (QoL) has grown. In response, the Cleveland Clinic team recently published an analysis of QoL among 563 adults who underwent mitral valve repair at their center via either sternotomy (n = 316) or a robotic approach (n = 247) from 2020 to early 2024 (JTCVS Open. 2025 Epub 10 Nov).
Patients in the robotic surgery group were younger and had fewer comorbidities and higher baseline QoL scores. The study found no significant difference in temporal outcomes through one year between the groups, with excellent postoperative QoL reported in both groups. QoL measures in both groups exceeded the population norm and returned to patients’ baseline levels within six months of surgery.
“These findings show that patients seeking mitral valve repair at an experienced center really can’t go wrong, regardless of the approach chosen,” Dr. Gillinov concludes. “At experienced centers, the choice for appropriate candidates for minimally invasive repair can and should be tailored to patient preference.”
Advertisement
Advertisement
NIH-funded comparative trial will complete enrollment soon
Why and how Cleveland Clinic achieves repair in 99% of patients
Two surgeons share insights on weighing considerations across the lifespan
An overview of growth in robot-assisted surgery, impressive re-repair success rates and more
Judicious application yields a 99.7% repair rate and 0.04% mortality
Cleveland Clinic series supports re-repair as a favored option regardless of failure timing
A call for surgical guidelines to adopt sex-specific thresholds of LV size and function
Cleveland Clinic series shows re-repair is feasible with excellent midterm results