High plasma ApoA1 and TG/HDL-C ratio predict faster progression
Plasma and cerebrospinal fluid (CSF) biomarkers of metabolic syndrome are associated with clinical outcomes in mild cognitive impairment (MCI) and Alzheimer’s disease (AD) dementia, suggesting their potential use for better predicting cognitive decline and as possible treatment targets. So asserts a team of Cleveland Clinic investigators in the first study to evaluate the association of metabolic syndrome biomarkers with longitudinal functional and cognitive decline in MCI and AD dementia. The study was published in Alzheimer’s Research & Therapy (2023;15:54).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Many biomarkers of metabolic syndrome are already routinely measured in clinical practice,” says the study’s lead and corresponding author, Jagan Pillai, MD, PhD, a staff neurologist with Cleveland Clinic Lou Ruvo Center for Brain Health in Cleveland. “Clarifying their role in cognitive decline may be important for recommending lifestyle changes and pharmacotherapy in a more timely manner to improve the course of MCI and AD.”
According to Dr. Pillai, disease course can vary widely among individuals with AD, and understanding the mechanisms underlying dementia progression may provide important clues to developing and promoting interventions to slow functional and cognitive decline.
Epidemiological studies have previously reported links between cognitive function and diabetes, metabolic syndrome and some cardiovascular disease risk factors. However, the precise relationships between clinical outcomes and key biomarkers of metabolic syndrome — including triglycerides (TG), high-density lipoprotein cholesterol (HDL-C) and apolipoprotein A1 (ApoA1; the key functional component of HDL) — have not been well characterized.
The study cohort consisted of 156 participants (106 with MCI, 50 with AD dementia) from the national Alzheimer’s Disease Neuroimaging Initiative research database. Overall, 63% were women, and the mean age was 74.9 (SD 7.3) years. Average follow-up was 4.0 (SD 2.8) years.
Plasma and CSF biomarkers were assessed at baseline and compared retrospectively with longitudinal changes in the Mini-Mental State Exam (MMSE), Clinical Dementia Rating – Sum of Boxes (CDR-SB) and Logical Memory delayed recall score.
Advertisement
Key findings included the following:
Dr. Pillai draws several conclusions from this study:
“Our studies support the hypothesis that metabolic syndrome disturbs the normal course of brain aging,” says Dr. Pillai. “This implies that reducing risk factors for metabolic syndrome may have important effects beyond diabetes and cardiovascular disease improvement, possibly in mitigating dementia onset.”
Advertisement
More about Dr. Pillai’s research in characterizing peripheral immune and blood-brain barrier changes in AD was recently summarized in a separate Consult QD article. His studies have been published in Annals of Clinical and Translational Neurology (2019;6[7]:1248-1262) and Frontiers in Aging Neuroscience (2021;13:676744).
Dr. Pillai is currently leading related investigations supported by a U.S. Department of Defense research award. His team is focusing on defining ApoA1 changes in patients with type 2 diabetes and preclinical AD, with the goal of clarifying ApoA1’s different roles in the peripheral and central nervous systems.
“Understanding this picture is critical to determining best management strategies,” he says. “We anticipate that this research will provide data to plan for future longitudinal studies evaluating targeted therapies against low plasma ApoA1 levels with the goal of reducing risk and progression of dementia among people with diabetes and those with early AD.”
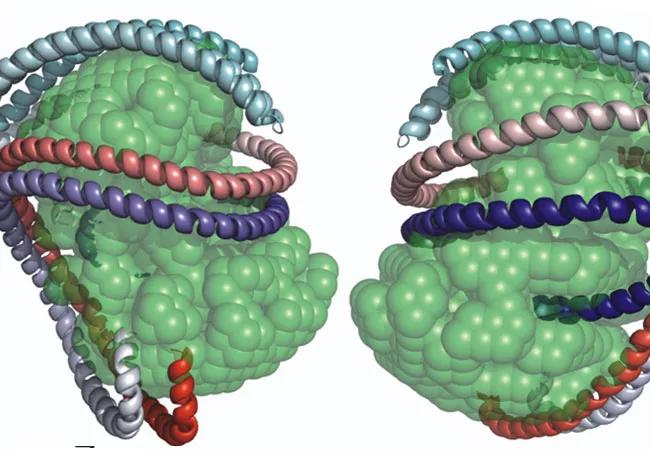
Image at top: Models of high-density lipoprotein with ApoA1 chains. Reprinted from the Journal of Biological Chemistry (2011;286[14]:12495-12508). ©The American Society for Biochemistry and Molecular Biology.
Advertisement
Advertisement

An expert talks through the benefits, limits and unresolved questions of an evolving technology

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Large NIH-funded investigation is exploring this understudied phenomenon

First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3

Observational evidence of neuroprotection with GLP-1 receptor agonists and SGLT-2 inhibitors

Machine learning study associates discrete neuropsychological testing profiles with neurodegeneration

Initial results show good accuracy of scalable, low-cost tool for flagging cognitive decline