ACC committee underscores need to properly weigh benefits in risk-benefit calculations

Many cardiologists are reluctant to prescribe hormone therapy (HT) to patients with symptoms of menopause because of concern about risks of cardiovascular disease (CVD). They may also be confused about recent evidence-based guidelines that support use of HT in certain situations.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To offer some clarity on risk/benefit considerations for menopausal HT from a cardiology perspective, the American College of Cardiology Cardiovascular Disease in Women Committee, led by Cleveland Clinic cardiologist Leslie Cho, MD, has issued a new in-depth review published in Circulation (2023;147:597-610). The paper offers guidance on practical implementation of guidelines from four major medical societies: the American College of Obstetricians and Gynecologists, the American Association of Clinical Endocrinology, the Endocrine Society and the North American Menopause Society.
“A lot of new information has emerged about HT since the Women’s Health Initiative results were first published, but there is a misconception among some clinicians that HT is horrible for every patient,” says Dr. Cho, Director of the Women’s Cardiovascular Center at Cleveland Clinic. “We believe it’s important for cardiologists to take a nuanced approach, and we hope this analysis will help them counsel their patients.”
The review includes perspective on the history of HT and CVD, information on the different forms of HT — systemic HT, transdermal estrogen and progestogens, compounded HT and vaginal estrogen therapy — and recommendations for HT use in specific subpopulations of women. Also covered are considerations for monitoring, discontinuation and extended use of HT, as well as which patients should generally avoid HT and noncardiovascular contraindications.
“The most important takeaway is that, based on evidence from 19 randomized controlled trials, HT is associated with a pretty low absolute risk of death, heart disease, myocardial infarction and angina,” says Dr. Cho. “However, we do need to be very careful about using it in women who have had deep venous thrombosis or who are at risk for stroke.”
Advertisement
Concern about excess cardiovascular risks associated with HT dates back to publication of results from the HERS (Heart and Estrogen/Progestin Replacement Study) and Women’s Health Initiative (WHI) trials. In the ensuing decades, with the accrual of additional evidence, a better understanding has emerged of when and how HT impacts a woman’s CVD risk.
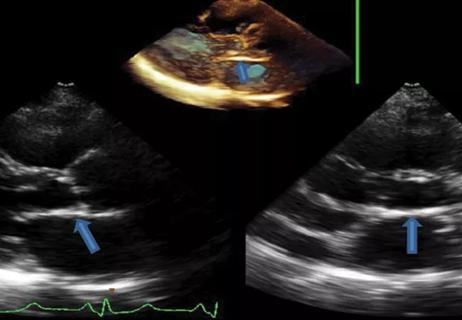
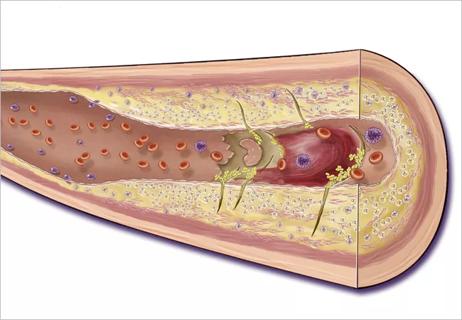
Age-stratified analyses of WHI data with median follow-up of 13 years showed that absolute risks of adverse events after HT initiation were much lower in women aged 50 to 59 than in those who were older and also lower in those who started taking HT within 10 years of menopause onset. These findings support the timing hypothesis — i.e., that CVD risk associated with HT may depend on when it is initiated relative to menopause onset. While HT may be safe for healthy women aged < 60 years or within 10 years of menopause onset, in the setting of advanced atherosclerosis, it may destabilize plaque and cause other adverse effects.
In keeping with the guidelines from the four medical societies, the ACC committee advises cardiologists to take a risk-stratified approach to HT, as follows:
Advertisement
“Because we believe coronary artery dissection is hormone-driven, patients with this condition should never take oral estrogen therapy,” says Dr. Cho. “It is also not appropriate for patients who have congenital heart disease or a history of thromboembolism, stroke or chronic obstructive pulmonary disease.”
For some patients — particularly those in the intermediate- or high-risk categories — transdermal estrogen and progestogens or vaginal estrogen may be a better choice than the oral route. Evidence from observational studies suggests that risk of VTE is lower with transdermal versus oral HT.
“There is a misconception that low-dose vaginal estrogen therapy is similar to oral HT in terms of risk,” Dr. Cho notes. “But that is not the case. Scientific evidence indicates that vaginal estrogen is not absorbed systemically.”
Even in lower-risk patients, cardiologists need to be mindful of HT’s potential impact on blood pressure and triglycerides. “It can mildly increase risk for hypertension,” Dr. Cho says, “and even a gain of 1 mmHg increases risk of stroke.”
The ACC committee urges cardiologists to adopt a shared decision-making approach when counseling patients about these issues. “Women who have had a stent or a heart attack are desperately afraid of taking any type of HT, and rightfully so,” Dr. Cho observes. “For women in the low- or intermediate-risk categories who are experiencing menopausal symptoms, a frank discussion is critical. Once they understand their risks and whether they can be controlled, these patients may be able to safely take hormones for their symptoms.”
Advertisement
“The clear winner in this updated review of treatment for vasomotor symptoms in menopause is transdermal formulations of HT,” says cardiologist Deirdre Mattina, MD, Medical Director of Cardio-Obstetrics at Cleveland Clinic Hillcrest Hospital, who was not involved in the review. “Across a range of low- and intermediate-risk patients, transdermal HT poses less risk than oral HT for unfavorable cardiovascular outcomes.
“Having a more in-depth understanding of the timing for initiation of HT and baseline patient risks for HT should provide cardiologists with the tools they need to help their patients make informed decisions,” Dr. Mattina adds.
Advertisement
Advertisement

Pediatric specialists unpack new evidence, considerations for care and what’s ahead
27th offering of this CME favorite to be held March 6-9 in Hollywood, Florida

Metabolites from animal product substrates implicated in heart failure development in community cohorts
Weakened endorsements in settings of normal EF and mild-moderate LV dysfunction may cause harm

AHA recommendations for pretransplant evaluation, peritransplant and long-term management

VMS in menopausal women can lead to adverse health outcomes

Newly identified pathway may explain the so-called niacin paradox

Giving young patients a hand as they take charge of their own health