It takes a multidisciplinary team to select candidates and optimize outcomes
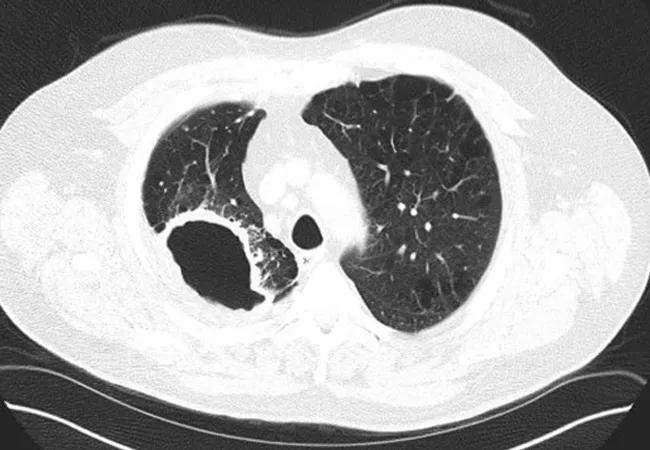
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b4117d1a-8af8-47a4-973b-d042d76fe2c0/21-PUL-2092113-Surgical-treatment-for-Mycobacterium-Avium-Complex-650X450_jpg)
21-PUL-2092113-Surgical treatment for Mycobacterium Avium Complex 650X450
Surgery is indeed a treatment option for select patients with Mycobacterium avium complex (MAC) pulmonary infection. Historically, surgical treatment was avoided, says pulmonologist Elliot Dasenbrook, MD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“There were a few reports of bad outcomes, which gave the impression that surgery for MAC may be ineffective or too risky,” he says. “But in a multidisciplinary program — with a pulmonologist who augments the ability of the lungs to clear out infection, an infectious disease specialist who optimizes the antibiotic therapy, a dietitian to work with malnutrition, and a surgeon who is highly experienced in lung resection — the outcomes are far better. It takes an expert team to select the patients most likely to benefit from surgery.”
The prevalence of MAC lung disease in the U.S. has increased significantly in the past 10-15 years as providers have become more aware of the disease and more likely to detect it through sputum culture or bronchoscopy as follow-up to an abnormal CT scan of the chest, notes Dr. Dasenbrook. MAC is the most common type of nontuberculous mycobacterial infection.
“The more we see and learn about MAC, the more we can confirm that there are a number of patients who would do very well with surgery,” he says.
Surgery may be indicated when medical therapy fails and/or there is recurring infection, antibiotic resistance or antibiotic intolerance, explains infectious disease specialist Cyndee Miranda, MD.
“It also may be indicated to eliminate or reduce symptoms, including life-threatening hemoptysis — even if there is residual disease present after resection,” says Dr. Miranda. “For some patients, debulking of the most severe parenchymal damage may slow disease progression to other areas.”
Advertisement
Even with the care of an expert team, only select patients with MAC infection are referred for surgery. In general, surgical candidates are patients with:
A pulmonary risk assessment, including clinical history and pulmonary function testing, is conducted for all surgical candidates. Risk of poor surgical outcomes is higher when forced expiratory volume in one second (FEV1) is less than 70%.
Patients with low body mass index (which is common in chronic pulmonary infection, notes Dr. Dasenbrook) are likely not surgical candidates due to poor nutritional status and inability to tolerate the procedure.
“Patients are typically on antibiotic treatment, with oral, intravenous or inhaled antibiotics, for around eight to 12 weeks before surgery,” says Dr. Miranda. “This attempt to decrease bacterial count in the sputum helps minimize perioperative complications. Some patients with refractory disease have been on MAC treatment for several months or even years prior to surgery.”
Advertisement
Preoperative interventions also include pulmonary rehabilitation, as moderate to intense exercise helps improve aerobic capacity, physical fitness and quality of life in patients scheduled for lung surgery. While this rehab occurs over an average of four to six weeks in lung cancer, patients have an opportunity for months of exercise therapy before surgery for MAC due to the infection’s slow progression.
The most common types of pulmonary resection to treat MAC infection are lobectomy and segmentectomy, says thoracic surgeon Daniel Raymond, MD. Other procedures include pneumonectomy, partial resection and wedge resection.
“Limited resection is generally associated with better outcomes,” he says.
Postoperatively, antibiotics are still continued for 12 months after sputum culture conversion to negative, adds Dr. Miranda. Long-term clearance rates of 95% at one year and 87% at three years after surgery have been reported. However, there are also postoperative complications to consider, with postoperative mortality ranging from 0% to 23% and postoperative morbidity ranging from 0% to 50%.
“Pulmonary resection can be an integral part of an effective treatment regimen for MAC infection,” concludes Dr. Dasenbrook. “The key is referring patients to a medical center that is experienced in treating MAC, with a multidisciplinary approach to selecting surgical candidates and optimizing them before and after surgery.”
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon
How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR
Optimal management requires an experienced center