Bimagrumab increases pelvic muscle volume in rat models
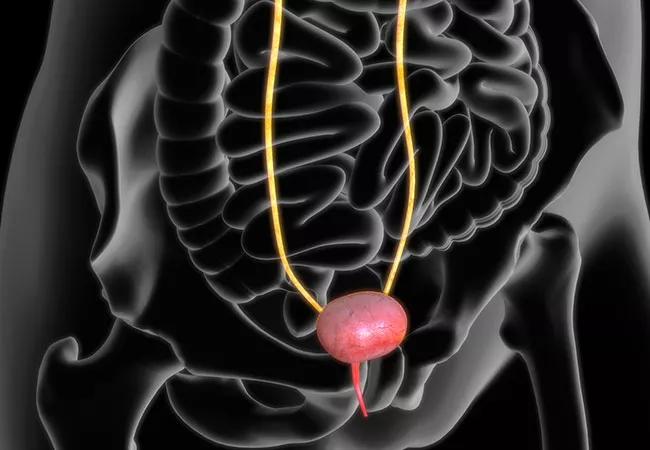
Bimagrumab, a novel myostatin inhibitor that enlarges muscle cells and builds muscle strength, has shown promise as a potential treatment for stress urinary incontinence (SUI). It’s the first muscle growth promoter to be studied for increasing urethral pressure and continence in an SUI model.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Currently, there are no medications available in the U.S. for treating SUI. Outside the U.S., treatments include pharmaceuticals that increase muscle tone, but none that increase muscle volume, like bimagrumab.
“Our lab study built on previous findings that SUI can be treated by increasing muscle tone of the urethra,” says Margot Damaser, PhD, a Cleveland Clinic biomedical researcher who focuses on female pelvic floor disorders. “Increasing muscle volume is another way to increase muscle tone and, therefore, muscle contraction.”
Results of the exploratory study by Dr. Damaser and her research team have been published in the American Journal of Physiology – Renal Physiology.
The study evaluated the effect of three drugs in rat models of SUI. The rats sustained pudendal nerve and pelvic muscle injury to mimic SUI. Then they received treatment with one of the following:
After two weeks, all three treatment groups had increases in body weight and muscle weight compared to the placebo group. But the most notable increase was in the bimagrumab group, which according to histology showed an approximately 10% increase in muscle weight.
“The rats’ dual injury included damaged nerve and muscle, which is hard to regenerate and can result in muscle atrophy,” says Dr. Damaser. “With bimagrumab, the rats’ pelvic muscles regenerated within two weeks of starting treatment.”
Advertisement
The drug also had a strong effect on extracellular matrix components, which made the healed muscle look nearly normal.
“Usually we see scarring when atrophied muscle heals, but that wasn’t the case with bimagrumab,” she says.
This proof-of-concept test is the first of many more preclinical studies needed before introducing a clinical trial. There are many unanswered questions about long-term effects of this treatment and proper dosage, says Dr. Damaser.
“We noted a gain in overall body weight with systemic bimagrumab,” she adds. “Would that be acceptable for patients with SUI? Or could we localize treatment, limiting it to just the urethra and pelvic floor?”
Even without these answers, this initial study hints that the future of SUI treatment could include pharmaceutical options, potentially filling the gap between conservative measures like lifestyle modifications and pelvic floor exercises, and more advanced therapies like collagen injections and surgery.
“Although other pharmaceuticals tested in the past 20 years have not been successful in the U.S., there may be other viable options,” says Dr. Damaser. “Our early results with bimagrumab open up a new category of drugs for further evaluation.”
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key