Case study in diagnosing ACNES and finding the right surgical fix
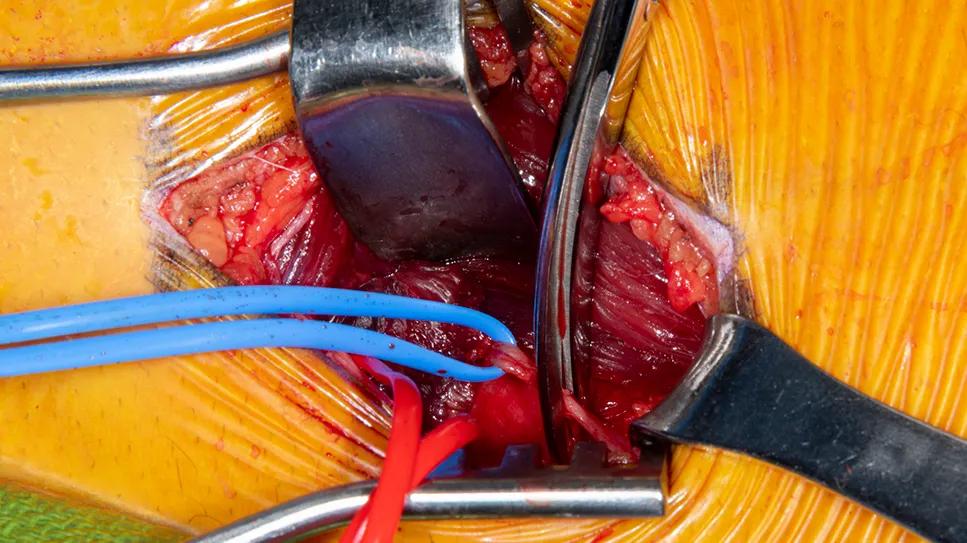
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1e85ca60-c1c9-4695-a9bf-bd2cb82b3b3b/peripheral-nerve-entrapment-syndrome-jack)
intraoperative view of nerve surgery
In January 2023, a 15-year-old female presented to Megan Jack, MD, PhD, a peripheral nerve neurosurgeon in Cleveland Clinic’s Neurological Institute, with severe abdominal pain that prevented her from going to school or engaging in normal activities.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The patient had had a two-year history of intermittent abdominal pain for which she had undergone workups by external providers without a clear diagnosis. The pain suddenly worsened in October 2022 without an inciting event. She was admitted to an outside hospital for testing and underwent abdominal ultrasonography and abdominal CT scanning. Laparoscopic appendectomy provided temporary relief from pain, but when the pain returned after three days, it was more localized and constant and caused nausea and vomiting.
When the patient presented at Cleveland Clinic, Dr. Jack suspected she might have anterior cutaneous nerve entrapment syndrome (ACNES), so she performed a Carnett’s test on the right lower quadrant of the abdomen. The test produced a sharp pain response, which confirmed the ACNES diagnosis. The patient was referred to Desimir Mijatovic, MD, an adult and pediatric pain management specialist in Cleveland Clinic’s Center for Spine Health, for identification of the affected nerves.
Dr. Mijatovic evaluated the patient and found tenderness over cutaneous nerves T10 and T11 on the right side of the abdomen. A nerve block at T11 produced 80% pain relief. The patient reported pain slightly higher in the abdomen, so a second nerve block was performed, at T10. This block produced 80% relief of the pain remaining after the first block. When the relief lasted only six hours — the duration of the local anesthetic — the patient was referred back to Dr. Jack for surgery.
In February 2023, Dr. Jack performed an anterior cutaneous nerve neurectomy on the patient’s intercostal nerves T9, T10 and T11. After locating each nerve at the lateral border of the rectus abdominis muscle where the nerves turn toward the skin, she cut the fascia of each entrapped nerve, releasing them and allowing retraction into the body.
Advertisement
The patient has been pain-free since the procedure. At her three-month checkup, she had discontinued pain medication, resumed her normal activities and returned to school.
ACNES occurs when cutaneous branches of the thoracoabdominal nerves become entrapped at the lateral border of the rectus abdominis, where they make a sharp turn toward the skin. The result is chronic abdominal pain that generally has both dull and sharp components.
Most patients with ACNES have no history of surgery, trauma, hernia, scar or other explanation for peripheral nerve entrapment. Patients are typically referred to a gastroenterologist or general surgeon to test for problems known to cause abdominal pain. When no explanation is found, Dr. Jack suggests thinking outside the box.
“It is important have a high clinical suspicion of ACNES when a patient has undergone a workup and there is no explanation for their ongoing abdominal pain, particularly if there has been no trauma or surgery,” she says.
ACNES is thought to be fairly rare, with reports suggesting it accounts for about 2% of emergency department visits for acute abdominal wall pain. The true prevalence is unknown, however, because it may be commonly overlooked when investigating cases of undifferentiated abdominal pain. “I see 10 to 20 cases a year, but it’s on my radar,” Dr. Mijatovic notes.
A Carnett’s test can be used to confirm the diagnosis. “I look for the location of the pain — most commonly in the lower right quadrant of the abdomen — and then put pressure on the area and ask the patient to sit up,” Dr. Jack explains. “A sharp pain response is considered a positive test and merits referral for identification of the nerves that are involved.”
Advertisement
Conservative treatment with pain medication, botulinum toxin or lidocaine injections may be tried. If these fail to bring sufficient relief, surgical management is indicated.
“The surgery is straightforward,” says Dr. Jack. “Permanent relief is the goal. The burning nerve pain should improve dramatically right away.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d5eca73b-306f-4ef2-a5e3-cc900fefd6e0/peripheral-nerve-entrapment-syndrome-inset1)
Figure. Intraoperative photo showing the anterior cutaneous nerve (surrounded by blue loop) deep to the rectus abdominis muscle just before neurectomy.
No physical therapy or other rehabilitative therapy is required after surgery. Lifting is initially limited to 10 pounds to prevent hernia development. After two weeks, heavier weights are gradually permitted.
Although the diagnosis of ACNES is relatively simple, most medical centers do not have the expertise required to treat the condition. Dr. Jack encourages physicians to contact her when no common explanation for chronic abdominal pain can be found.
“Refer the patient on to let them get their life back,” she says.
Advertisement
Advertisement
Researchers seek solutions to siloed care, missed diagnoses and limited access to trauma-informed therapies
Cleveland Clinic study investigated standard regimen
Program participation correlates with reduced use of opioids, X-rays and ED visits
Researchers identify the neurologic evolution of pain-related learning
Tapping into motivational interviewing to guide behavioral change
This common condition remains tough to work up and diagnose, and treatment options are limited
Self-efficacy mindset, burst therapy and increased biofeedback may help improve outcomes
How functional restoration can help children with these conditions marked by unexplained pain with stigmatized symptoms