For now, antibody testing is recommended only when considering an alternative diagnosis
By Albert Aboseif, DO; J. Daniel Bireley, MD; Yuebing Li, MD, PhD; David Polston, MD; and Justin R. Abbatemarco, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Note: This article is reprinted from the Cleveland Clinic Journal of Medicine (2023;90[7)]:439-447).
Postural orthostatic tachycardia syndrome (POTS) is a common form of orthostatic intolerance, with a prevalence of 0.2% to 1% in developed countries.1 While no single unifying etiologic mechanism has been determined, several have been proposed, including activation of the immune system.1–3
In this review, we describe the presentation and diagnostic evaluation of POTS for the general practitioner, including atypical features that may suggest an alternative diagnosis requiring a more extensive evaluation. We also touch briefly on its basic treatment, possible autoimmune mechanisms (including recently associated antibody targets and their clinical utility), immunosuppressive therapy and future directions in the field.
POTS is a chronic syndrome defined by a sustained increase in heart rate of at least 30 beats per minute (bpm) within 10 minutes of standing in adults (or ≥ 40 bpm in patients ages 12 to 19) without accompanying orthostatic hypotension, which is defined as a fall in systolic blood pressure of 20 mmHg or greater or a fall in diastolic blood pressure of 10 mmHg or greater (Table 1).1,2,4,5 In many patients, the absolute heart rate while upright remains above 120 bpm.
POTS symptoms can be grouped broadly as either cardiovascular or noncardiovascular (Table 2).1 Orthostatic intolerance is a defining feature of the condition, with symptoms that get worse upon standing and improve with supine posture.5 Additional cardiovascular symptoms include palpitations, dizziness, lightheadedness, and presyncope or syncope. Noncardiovascular symptoms can involve many organ systems and include fatigue, generalized weakness, neuropathic pain, cognitive difficulty, nausea and bladder dysfunction (Table 3).1,5–7
Advertisement
The onset is typically subacute and often follows a trigger such as infection, surgery, trauma, or childbirth.6 Heat, fever, dehydration, morning hours, strong emotion and menstruation have been known to exacerbate symptoms.1 The typical age at onset is between 15 and 45, and at least 80% of patients are women.1,2,6
A typical presentation of POTS is in a young active woman with a subacute onset of lightheadedness, dizziness and presyncope provoked by standing, often following a viral illness, surgical procedure, trauma or prolonged period of inactivity. The patient may report that symptoms are worse in warm weather or morning hours, or when he or she is feeling particularly stressed or anxious.1
A unifying pathophysiology of POTS has not been determined, although various mechanisms may be involved. These include abnormally increased sympathetic nervous system activity and circulating catecholamines resulting in a hyperadrenergic state (“hyperadrenergic POTS”), peripheral sympathetic denervation leading to venous pooling and volume dysregulation (“neuropathic POTS”), low blood volume (absolute hypovolemia) and an underlying immune dysregulation (discussed in further detail below).1–3
These varying mechanisms may coexist within an individual patient, resulting in a heterogeneous symptom presentation, ultimately defined by orthostatic intolerance.5
POTS can be diagnosed clinically by the general practitioner without extensive testing.8 However, lack of familiarity with the condition, its nonspecific symptoms indirectly related to orthostatic intolerance and the overlap of symptoms with those of similar conditions often result in unnecessary referrals, excessive testing and a delay in diagnosis, as concern about missing an alternative diagnosis often adds to the diagnostic challenge.9,10
Advertisement
Using the clinical history alone, POTS can be challenging to differentiate from other causes of orthostatic intolerance such as chronic fatigue syndrome and inappropriate sinus tachycardia.10 Fortunately, objective testing can help identify POTS, and the initial management strategies are often similar.10 Further information on differentiating POTS from other causes of orthostatic intolerance can be found elsewhere.5
Comorbid psychiatric conditions such as untreated major depression can complicate the evaluation but are important to recognize and address in equal measure to improve clinical response to treatment.11
The diagnostic evaluation of POTS starts with a focused history centering on symptom onset and progression, comorbid conditions, precipitating and exacerbating factors, and positional dependence. Other topics and investigations include the following:
Advertisement
Further investigation, including ancillary cardiovascular testing (echocardiography, external electrocardiographic loop monitoring), is not recommended as part of the routine evaluation unless there is strong suspicion for structural heart disease or symptomatic arrhythmia contributing to exercise intolerance.4 Similarly, tilt-table testing is not required for diagnosis but can be useful when a patient is unable to perform an active stand test or when other conditions, such as neurocardiogenic (vasovagal) syncope or peripheral autonomic neuropathy, are suspected.7,16
Further autonomic testing — such as quantitative sudomotor axonal reflex testing, skin biopsy to evaluate epidermal nerve fiber density, thermoregulatory sweat testing or other autonomic cardiovascular evaluation (e.g., Valsalva maneuver, deep-breathing test) — is unnecessary for the initial diagnosis. These tests may be pursued by a specialist primarily to understand the underlying pathophysiology of a particular patient who has had no improvement with initial conventional therapy, and when symptoms raise suspicion for an autonomic neuropathy.5
Nonpharmacologic treatments first
Once the diagnosis of POTS is established, initial treatment is aimed at reducing symptoms, improving quality of life and educating the patient. Nonpharmacologic strategies should be the first intervention and include the following:
Advertisement
An in-depth discussion of treatment for patients with severe or refractory symptoms is beyond the scope of this article but can be found elsewhere.19
In evaluating a putative POTS diagnosis, it is important to recognize certain red-flag features (outlined below) that may suggest an alternative diagnosis. When these features are present, a more thorough workup should be considered.
Evolving symptoms, with widespread dysautonomia that is highly debilitating and rapidly progresses over days to weeks, should raise concern for an alternative diagnosis.14,20
A history of autoimmune disease or malignancy may further raise suspicion for an alternative diagnosis, especially if the initial presentation occurs after age 65.20
Red-flag autonomic symptoms are often widespread and severe, involving the sympathetic, parasympathetic and enteric nervous systems. Signs and symptoms that should raise suspicion include pupillary dysfunction, hyperhidrosis or anhidrosis, urinary retention, sexual dysfunction and severe gastrointestinal dysmotility.14 The coexistence of these symptoms should raise suspicion for an alternative diagnosis, especially when disabling and severe.
Extra-autonomic features that should also raise concern for alternative diagnoses include involvement of the central nervous system (cerebral cortex, brainstem, cerebellum, spinal cord) or endocrinopathies (amenorrhea, syndrome of inappropriate antidiuretic hormone secretion, adrenal insufficiency, panhypopituitarism).14
If red flags are present
When red-flag features are present, systemic testing and/or neurologic testing may be warranted. In these cases, testing for specific antibodies that could account for the clinical presentation is advised.
For example, a combination of sicca symptoms, impaired pupillary reflex, urinary retention and gastroparesis should raise suspicion for a severe form of immune-mediated dysautonomia termed autoimmune autonomic ganglionopathy.20 This clinical picture warrants testing for the alpha-3 ganglionic acetylcholine receptor (gAChR) antibody.20
A limited form of autoimmune autonomic ganglionopathy that predominantly affects the gastrointestinal system is termed autoimmune gastrointestinal dysmotility syndrome.21 Patients with this form develop severe subacute multilevel gastrointestinal dysmotility, sometimes presenting with intestinal pseudo-obstruction, and are often found to be gAChR antibody-positive.21
Alternatively, predominant sicca symptoms in the setting of dysautonomia with or without sensory abnormalities may warrant testing for Sjögren syndrome A and B (SSA and SSB) antibodies.22,23
Patients who present with dysautonomia in the setting of symmetric proximal weakness that improves with exercise should raise suspicion for Lambert-Eaton myasthenic syndrome and should undergo testing for P/Q-type and N-type voltage-gated calcium channel antibodies.20
Other antibody-associated (often paraneoplastic) neurologic disorders exist that can present with pervasive dysautonomia, often in the setting of severe nervous system dysfunction. They are beyond the scope of this review, but include disorders associated with antineuronal nuclear antibody type 1 (ANNA-1, Anti-Hu), anti-dipeptidyl-peptidase-like protein-6, anti-contactin-associated protein-like 2 antibody, and anti-collapsin response mediator protein 5.20,24 They are rare and should not be tested for regularly unless clinically indicated, to avoid exposing patients to unnecessary and potentially harmful interventions.
The overlap of signs and symptoms among several of these autoimmune conditions and POTS has raised the possibility of an underlying autoimmune mechanism in the disease itself. The following section focuses on this topic in greater detail.
The role of the immune system in POTS has attracted much interest in recent years. While a clear autoimmune etiology has not been identified, the shared clinical features between POTS and various autoimmune conditions suggest several immune-mediated mechanisms. These shared features have also given rise to further investigation into possible diagnostic and management avenues within the field.
Clinical similarities between POTS and autoimmune conditions
Most patients with POTS are young women, with recent estimates suggesting a 94% female predominance.25 Symptom onset is frequently preceded by an acute stimulus such as a viral infection, vaccination, physical trauma, surgery or pregnancy, suggesting an immune-mediated process may be at play.25 Furthermore, many patients with POTS have associated generalized symptoms including fatigue, malaise, sleep disruption, headache and gastrointestinal symptoms, features often observed in chronic autoimmune disease.25
From 16% to 20% of patients with POTS have a coexisting autoimmune disease, and many have a family history of one.9,26,27 In a large community-based survey, the most common coexisting autoimmune conditions were Hashimoto thyroiditis (present in 6%), celiac disease (3%), Sjögren syndrome (3%), rheumatoid arthritis (2%) and systemic lupus erythematosus (2%).9
Furthermore, many patients with POTS have various autoantibodies, suggesting an autoimmune link. However, many of these antibodies are discovered incidentally at low titers and have unclear clinical significance.26,28,29 One study found that 25 (25%) of 100 patients with POTS had antinuclear antibodies, significantly more than in the general population (16%, P < 0.05).26 Similarly, the prevalence of anti-phospholipid antibodies in the patients with POTS was 7%, compared with 1% in the general population (P < 0.001).26 Thyroid-specific antibodies have also been found in up to 33% of patients with POTS, again with unclear significance.30 Neurologic autoantibodies directed at voltage-gated potassium channels and glutamic acid decarboxylase 65 may also be incidentally discovered but are nonspecific, and can also be seen in patients with nonimmune neurologic diseases as well as in healthy controls.28
While the prevalence of antibody positivity in patients with POTS may suggest an autoimmune association, the presence of these antibodies shows no clear difference in the severity of POTS symptoms or response to therapy. In clinical practice, checking for these antibodies is not recommended in patients with an otherwise typical POTS presentation without additional features of an underlying secondary disease process.26,28
Certain autoimmune conditions may also feature POTS-like symptoms, further complicating the diagnosis and signifying an important autoimmune parallel. For example, milder cases of Sjögren syndrome can resemble POTS.22 Neurologic involvement of Sjögren syndrome can classically cause a subacute sensory ganglionopathy with debilitating autonomic features.31 However, a milder form of Sjögren syndrome can present with predominant sicca symptoms (dry mouth, dry eyes) and mild autonomic symptoms due to an underlying small-fiber neuropathy.22
Goodman et al22 reported a series of 13 patients with Sjögren syndrome who underwent evaluation for suspected autonomic impairment, finding that eight met the criteria for POTS based on clinical features and autonomic testing. Importantly, all 13 patients had sicca symptoms at onset, and most had a combination of elevated SSA and SSB antibodies or pathologic findings on salivary gland biopsy, suggesting that only patients with autonomic features in conjunction with clear Sjögren syndrome symptoms warrant antibody testing.
Molecular mechanisms proposed
The molecular mechanisms linking POTS and autoimmunity remain poorly understood. One theory suggests a state of sympathetic overdrive and reduction of cardiovagal tone resulting in an elevation in the cytokine interleukin 6 inducing systemic inflammation.32 The elevation in interleukin 6 may act centrally to upregulate further sympathetic activity, resulting in a chronic hyperadrenergic state leading to cardiovascular deconditioning.32 This proinflammatory state may explain several systemic features associated with POTS, including sleep disturbance, cognitive impairment and hyperalgesia.32 Additionally, elevated cytokines may be important mediators of vasodilation and vascular permeability.33
Others have suggested the possibility of a circulating autoantibody with a direct pathological mechanism affecting the autonomic nervous system.34
To date, several possible autoantibody targets have been studied in POTS.
The gAChR antibody, initially identified as the pathogenic antibody in autoimmune autonomic ganglionopathy, has been suggested as a possible culprit,35 as it can be detected in low titers in up to 25% of patients with POTS.6,36 However, it can be nonspecific, as low-titer positivity (≤ 0.05 nmol/L) has been noted in healthy controls and in various other autoimmune-mediated conditions, without clear clinical relevance.29 While the antibody has been speculated to play a role in sympathetic denervation in POTS, no clear clinical difference between seropositive and seronegative patients has been shown.6,36,37 Thus, it is always important to interpret antibody testing results within the clinical context, regardless of the titer level. Ultimately, testing for gAChR antibody in a patient with a classic POTS presentation without additional red flags has little clinical utility and may confound the clinical picture if the result is positive.37
G-protein coupled receptor (GPCR) antibodies, which target adrenergic receptors, are another class of antibodies that may be detected in patients with POTS.34 Notably, GPCR antibodies have also been detected in patients with Sjögren syndrome, orthostatic hypotension, malignant hypertension and preeclampsia, as well as in patients with POTS-like conditions such as inappropriate sinus tachycardia, complex regional pain syndrome and chronic fatigue syndrome, and are thus nonspecific.25 Specific antibodies in this class include those directed against alpha-1 adrenergic receptor, beta-1 adrenergic receptor and beta-2 adrenergic receptor and are thought to inhibit norepinephrine action peripherally, resulting in increased heart rate and orthostatic intolerance.34
Angiotensin II T1 receptor antibodies have similarly been detected in patients with POTS and may act by disrupting systemic vasoconstriction in response to upright posture.38
Muscarinic receptor antibodies. Recent evidence has also suggested activity of muscarinic receptor antibodies (M1, M2) in contributing to POTS pathophysiology.39
Testing for these antibodies is currently considered experimental and thus is not available commercially. Furthermore, a recent study investigating the presence of GPCR antibodies in POTS patients compared with healthy controls showed no significant difference in antibody (adrenergic, muscarinic, and angiotensin II) concentrations by enzyme-linked immunosorbent assay testing.40 While the presence of these antibodies raises the possibility of an autoimmune link, they do not appear to be directly pathogenic, and testing for them does not currently offer clear clinical utility in POTS.34,40
Given the possibility of an immune-mediated mechanism underlying POTS, researchers have begun to investigate the efficacy of immunotherapies in its treatment, but no prospective trials have yet been completed.
In a case series from Rodriguez and colleagues,41 six patients with a clinical diagnosis of POTS and a positive GPCR antibody test were treated with intravenous immunoglobulin intermittently over six months. All patients were young women (ages 23-31), had refractory POTS symptoms despite first-line treatment and had tested positive for the alpha-1 adrenergic receptor antibody. Response to treatment was measured with a subjective symptom-based survey and objective testing including a tilt-table test. The subjective and objective results appeared to be positive after six months of therapy, although treatment tolerance was poor, with two patients requiring hospitalization. Also, all patients were pretreated with intravenous fluids in addition to receiving intravenous immunoglobulin, likely resulting in a significant volume repletion that may have contributed to the overall treatment effect. This is an important confounder in assessing the use of intravenous immunoglobulin in the treatment of POTS.
Currently, a double-blind randomized controlled trial is investigating the feasibility, tolerability and potential benefit of intravenous immunoglobulin treatment in POTS.42 The study plans to enroll 32 participants with POTS who have moderate to severe symptoms and clinical or laboratory features of autoimmunity including a serum autoantibody (antinuclear antibody, gAChR antibody, extractable nuclear antigen, antiphospholipid antibody or tissue transglutaminase immunoglobulin A), a personal or family history of autoimmune disease, evidence of small-fiber neuropathy, or a history of acute to subacute onset of symptoms. With an expected completion date in late 2023, this study will help further clarify a clinical question that currently remains uncertain. Until then, there is not enough rigorous evidence to suggest a benefit of immunotherapy in the treatment of POTS.
Although the etiology and pathophysiologic mechanisms underlying POTS remain uncertain, a clinical diagnosis can be made with a focused history, examination and basic diagnostic evaluation.
Initial treatment strategies are simple and include optimizing fluid intake, compression stockings, avoidance of known triggers, exercise to improve stamina and cognitive behavioral therapy to reduce hypervigilance.
Autoimmunity may play a role in the pathogenesis of POTS in some patients. However, if the initial clinical presentation is consistent with POTS and no major red-flag features are evident, further antibody testing is not recommended because it will not change management. Although several antibodies are being investigated that may be associated with POTS, a single causative antibody has not been identified. If red flags are present, a targeted autoimmune investigation should be considered to exclude diagnostic mimics.
There are not enough data currently to warrant treating POTS with immunosuppressive therapies. Important clinical trials are underway to explore this treatment approach further.
Dr. Li reports serving as member of a clinical practice scientific advisory board and as research principal investigator for Alexion; consulting, serving as a research principal investigator, and receiving grant support from Argenx; consulting, serving as a research principal investigator for Catalyst and UCB; and serving as an advisor or review panel participant and serving as principal investigator in an upcoming trial for Immunovant. Dr. Abbatemarco reports consulting for Alexion; serving as an advisor or review panel participant for Genentech and EMD Serono and Horizon Therapeutics; and receiving a research grant from Horizon Therapeutics. The other authors report no relevant financial relationships that could be perceived as a potential conflict of interest in the context of their contributions to this article.
1. Fedorowski A. Postural orthostatic tachycardia syndrome: clinical presentation, aetiology and management. J Intern Med. 2019;285(4):352-366. doi:10.1111/joim.12852
2. Sheldon RS, Grubb BP 2nd, Olshansky B, et al. 2015 Heart Rhythm Society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015;12(6):e41-e63. doi:10.1016/j.hrthm.2015.03.029
3. Vernino S, Bourne KM, Stiles LE, et al. Postural orthostatic tachycardia syndrome (POTS): state of the science and clinical care from a 2019 National Institutes of Health expert consensus meeting—part 1. Auton Neurosci. 2021;235:102828. doi:10.1016/j.autneu.2021.102828
4. Freeman R, Wieling W, Axelrod FB, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton Neurosci. 2011;161(1-2):46-48. doi:10.1016/j.autneu.2011.02.004
5. Raj SR, Guzman JC, Harvey P, et al. Canadian Cardiovascular Society position statement on postural orthostatic tachycardia syndrome (POTS) and related disorders of chronic orthostatic intolerance. Can J Cardiol. 2020;36(3):357-372. doi:10.1016/j.cjca.2019.12.024
6. Thieben MJ, Sandroni P, Sletten DM, et al. Postural orthostatic tachycardia syndrome: the Mayo Clinic experience. Mayo Clin Proc. 2007;82(3):308-313. doi:10.4065/82.3.308
7. Deb A, Morgenshtern K, Culbertson CJ, et al. A survey-based analysis of symptoms in patients with postural orthostatic tachycardia syndrome. Proc (Bayl Univ Med Cent). 2015;28(2):157-159. doi:10.1080/08998280.2015.11929217
8. Bryarly M, Phillips LT, Fu Q, et al. Postural orthostatic tachycardia syndrome: JACC focus seminar. J Am Coll Cardiol. 2019;73(10):1207-1228. doi:10.1016/j.jacc.2018.11.059
9. Shaw BH, Stiles LE, Bourne K, et al. The face of postural tachycardia syndrome—insights from a large cross-sectional online community-based survey. J Intern Med. 2019;286(4):438-448. doi:10.1111/joim.12895
10. Olshansky B, Cannom D, Fedorowski A, et al. Postural orthostatic tachycardia syndrome (POTS): a critical assessment. Prog Cardiovasc Dis. 2020;63(3):263-270. doi:10.1016/j.pcad.2020.03.010
11. Anderson JW, Lambert EA, Sari CI, et al. Cognitive function, health-related quality of life, and symptoms of depression and anxiety sensitivity are impaired in patients with the postural orthostatic tachycardia syndrome (POTS). Front Physiol. 2014;5:230. doi:10.3389/fphys.2014.00230
12. Abed H, Ball PA, Wang LX. Diagnosis and management of postural orthostatic tachycardia syndrome: a brief review. J Geriatr Cardiol. 2012;9(1):61-67. doi:10.3724/SP.J.1263.2012.00061
13. Green EA, Raj V, Shibao CA, et al. Effects of norepinephrine reuptake inhibition on postural tachycardia syndrome. J Am Heart Assoc. 2013;2(5):e000395. doi:10.1161/JAHA.113.000395
14. Nakane S, Mukaino A, Higuchi O, et al. Autoimmune autonomic ganglionopathy: an update on diagnosis and treatment. Expert Rev Neurother. 2018;18(12):953-965. doi:10.1080/14737175.2018.1540304
15. Plash WB, Diedrich A, Biaggioni I, et al. Diagnosing postural tachycardia syndrome: comparison of tilt testing compared with standing haemodynamics. Clin Sci (Lond). 2013;124(2):109-114. doi:10.1042/CS20120276
16. Cheshire WP Jr., Goldstein DS. Autonomic uprising: the tilt table test in autonomic medicine. Clin Auton Res. 2019;29(2):215-230. doi:10.1007/s10286-019-00598-9
17. Bourne KM, Sheldon RS, Hall J, et al. Compression garment reduces orthostatic tachycardia and symptoms in patients with postural orthostatic tachycardia syndrome. J Am Coll Cardiol. 2021;77(3):285-296. doi:10.1016/j.jacc.2020.11.040
18. Fu Q, Levine BD. Exercise and non-pharmacological treatment of POTS. Auton Neurosci. 2018;215:20-27. doi:10.1016/j.autneu.2018.07.001
19. Kichloo A, Aljadah M, Grubb B, Kanjwal K. Management of postural orthostatic tachycardia syndrome in the absence of randomized controlled trials. J Innov Card Rhythm Manag. 2021;12(7):4607-4612. doi:10.19102/icrm.2021.120705
20. Mckeon A, Benarroch EE. Autoimmune autonomic disorders. Handb Clin Neurol. 2016;133:405-416. doi:10.1016/B978-0-444-63432-0.00022-0
21. Dhamija R, Tan KM, Pittock SJ, et al. Serologic profiles aiding the diagnosis of autoimmune gastrointestinal dysmotility. Clin Gastroenterol Hepatol. 2008;6(9):988-992. doi:10.1016/j.cgh.2008.04.009
22. Goodman BP, Crepeau A, Dhawan PS, et al. Spectrum of autonomic nervous system impairment in Sjögren syndrome. Neurologist. 2017;22(4):127-130. doi:10.1097/NRL.0000000000000134
23. Goodman BP. Evaluation of postural tachycardia syndrome (POTS). Auton Neurosci. 2018;215:12-19. doi:10.1016/j.autneu.2018.04.004
24. Neal AJ, Qian MY, Clinch AS, Le BH. Orthostatic hypotension secondary to CRMP-5 paraneoplastic autonomic neuropathy. J Clin Neurosci. 2014;21(5):885-886. doi:10.1016/j.jocn.2013.07.035
25. Vernino S, Stiles LE. Autoimmunity in postural orthostatic tachycardia syndrome: current understanding. Auton Neurosci. 2018;215:78-82. doi:10.1016/j.autneu.2018.04.005
26. Blitshteyn S. Autoimmune markers and autoimmune disorders in patients with postural tachycardia syndrome (POTS). Lupus 2015; 24(13):1364-1369. doi:10.1177/0961203315587566
27. Boris JR, Huang J, Shuey T, Bernadzikowski T. Family history of associated disorders in patients with postural tachycardia syndrome. Cardiol Young. 2020;30(3):388-394. doi:10.1017/S1047951120000165
28. McKeon A, Lennon VA, Lachance DH, et al. Ganglionic acetylcholine receptor autoantibody: oncological, neurological, and serological accompaniments. Arch Neurol. 2009;66(6):735-741. doi:10.1001/archneurol.2009.78
29. Li Y, Jammoul A, Mente K, et al. Clinical experience of seropositive ganglionic acetylcholine receptor antibody in a tertiary neurology referral center. Muscle Nerve. 2015;52(3):386-391. doi:10.1002/mus.24559
30. Singer W, Klein C, Low P, Lennon V. Autoantibodies in the postural tachycardia syndrome (P1.272) [abstract]). Neurology. 2015;84(suppl 14):P1.272.
31. Gwathmey KG. Sensory neuronopathies. Muscle Nerve. 2016;53(1):8-19. doi:10.1002/mus.24943
32. Okamoto LE, Raj SR, Gamboa A, et al. Sympathetic activation is associated with increased IL-6, but not CRP in the absence of obesity: lessons from postural tachycardia syndrome and obesity. Am J Physiol Heart Circ Physiol. 2015;309(12):H2098-H2107. doi:10.1152/ajpheart.00409.2015
33. Pavlov VA, Tracey KJ. The vagus nerve and the inflammatory reflex — linking immunity and metabolism. Nat Rev Endocrinol. 2012;8(12):743-754. doi:10.1038/nrendo.2012.189
34. Fedorowski A, Li H, Yu X, et al. Antiadrenergic autoimmunity in postural tachycardia syndrome. Europace. 2017;19(7):1211-1219. doi:10.1093/europace/euw154
35. Vernino S, Low PA, Fealey RD, et al. Autoantibodies to ganglionic acetylcholine receptors in autoimmune autonomic neuropathies. N Engl J Med. 2000;343(12):847-855. doi:10.1056/NEJM200009213431204
36. Sandroni P, Low PA. Other autonomic neuropathies associated with ganglionic antibody. Auton Neurosci. 2009;146(1-2):13-17. doi:10.1016/j.autneu.2008.10.022
37. Bryarly M, Raj SR, Phillips L, et al. Ganglionic acetylcholine receptor antibodies in postural tachycardia syndrome. Neurol Clin Pract. 2021;11(4):e397-e401. doi:10.1212/CPJ.0000000000001047
38. Yu X, Li H, Murphy TA, et al. Angiotensin II type 1 receptor autoantibodies in postural tachycardia syndrome. J Am Heart Assoc. 2018;7(8):e008351. doi:10.1161/JAHA.117.008351
39. Dubey D, Hopkins S, Vernino S. M1 and M2 muscarinic receptor antibodies among patients with postural orthostatic tachycardia syndrome: potential disease biomarker [abstract]. J Clin Neuromuscul Dis. 2016;17:S-9.
40. Hall J, Bourne KM, Vernino S, et al. Detection of G protein-coupled receptor autoantibodies in postural orthostatic tachycardia syndrome using standard methodology. Circulation. 2022;146(8):613-622. doi:10.1161/CIRCULATIONAHA.122.059971
41. Rodriguez B, Hoepner R, Salmen A, et al. Immunomodulatory treatment in postural tachycardia syndrome: a case series. Eur J Neurol. 2021;28(5):1692-1697. doi:10.1111/ene.14711
42. US National Institutes of Health. IVIG (Gamunex-C) Treatment Study for POTS Subjects (iSTAND). ClinicalTrials.gov identifier: NCT03919773. https://clinicaltrials.gov/ct2/show/NCT03919773. Accessed June 12, 2023.
Dr. Aboseif was an adult neurology resident at Cleveland Clinic when this article was written. Dr. Bireley is a current adult neurology resident at Cleveland Clinic. Drs. Li, Polston and Abbatemarco are staff neurologists at Cleveland Clinic.
Advertisement

Guidance from an expert on distinguishing — and co-managing — the disorders

Despite less overall volume loss than in MS and NMOSD, volumetric changes correlate with functional decline

It’s time to get familiar with this emerging demyelinating disorder

From dryness to diagnosis
Early experience with the agents confirms findings from clinical trials
Early data show risk is 73% higher in patients with lupus, 40% higher in patients with rheumatoid arthritis

Despite advancements, care for this rare autoimmune disease is too complex to go it alone
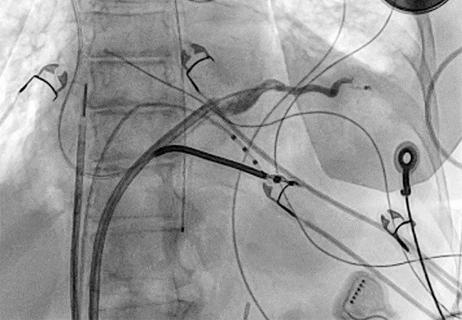
Procedure allows for safer epicardial VT mapping and ablation