Researchers refining computer program for greater accuracy
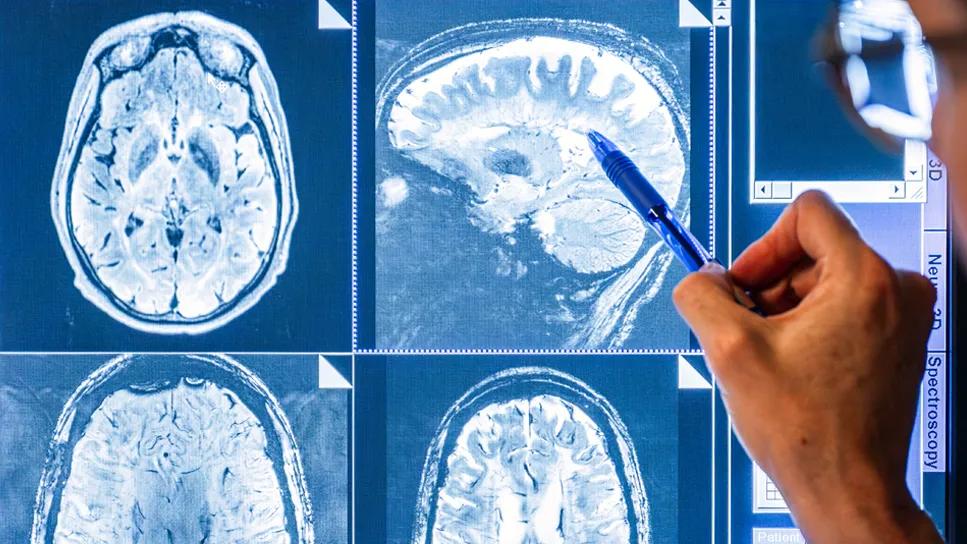
Oncologists often struggle to distinguish radiation-induced treatment effects from tumor recurrence in brain metastasis patients when looking at follow-up MRIs after radiosurgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Both conditions have similar morphological appearances on an MRI, and the patients can also exhibit similar symptoms: edema, memory loss, cognitive difficulties, seizures. The treatment for radiation necrosis (RN), however, is far less invasive than the treatment for tumor regrowth.
“It’s very challenging to distinguish between the two,” says Jennifer Yu, MD, PhD, Department of Radiation Oncology and Department of Stem Cell Biology and Regenerative Medicine. “And the dilemma that we as doctors face is: Should we go ahead and retreat the patient for tumor recurrence? Or do we give steroids to the patient to treat radiation necrosis?”
Dr. Yu and Pallavi Tiwari, PhD, assistant professor of biomedical engineering at Case Western Reserve University, hope to make it easier for radiation oncologists to read those MRIs through a machine learning project that uses an algorithm to distinguish between the two conditions.
“The idea is based on the fact that tumors have more chaos, more entropy,” says Dr. Yu. “You might be able to detect these subtle changes in entropy, which is higher in true tumor progression compared to radiation necrosis.”
Patients with brain metastases frequently are treated by stereotactic radiosurgery, which offers excellent tumor control but can also cause RN.
Because it is difficult to distinguish between tumor recurrence and RN on an MRI, as many as 20 to 40 percent of all patients are subjected to multiple radiological studies, brain lesion biopsies and even resections for what is ultimately deemed RN. Brain biopsy is currently the only definitive test to determine whether an MRI image is RN or tumor recurrence, but such procedures comes with a cost. Brain biopsies are risky, often causing morbidity and mortality.
Advertisement
“We really need a less invasive method for distinguishing these two conditions,” Dr. Yu says.
Although both radiation necrosis and tumor recurrence appear similar on an MRI, studies have shown that the underlying biological pathways are fundamentally different. The researchers reasoned that there would be phenotypic differences that, while not easily seen by the human eye, could be found on MRIs and used to distinguish the two.
Dr. Tiwari’s team first used an algorithm to extract quantitative features from MRIs then trained a computer algorithm program to identify the features that discriminate between cancer and RN. They used follow-up MRI scans from 43 patients.
The program, which Tiwari’s group named Co-occurrence of Local Anisotropic Gradient Orientations or CoLlAGe, looks at the edges of each pixel in the image captured in an MRI to see if they point the same way or in different directions. The latter indicates chaos, the hallmark of a tumor and not RN.
Now Drs. Tiwari and Yu are co-principal investigators on a new study, funded by a three-year Dana Foundation grant, that will evaluate and refine CoLlAGe. They will evaluate MRIs from patients treated at Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center.
Preliminary studies have shown the algorithm can improve neuroradiologists’ accuracy in interpreting the MRIs from 40-50 percent to 80 percent, Dr. Yu says. “And we’d like to make it even more accurate.”
Dr. Yu expects the computer program would be used to support neuroradiologists in improving their confidence in identifying a suspicious lesion as radiation necrosis or cancer recurrence.
Advertisement
“By having this extra tool, neuroradiologists and other physicians will feel more confident in their diagnoses,” says Dr. Yu, “and will be able to treat patients for either RN or a recurrent tumor more efficiently.”
Advertisement
Advertisement

First full characterization of kidney microbiome unlocks potential to prevent kidney stones

Researchers identify potential path to retaining chemo sensitivity

Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests

Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology