Going beyond the Eckardt symptom score to evaluate dyspepsia, eating and symptom “bother”

Cleveland Clinic researchers have developed and validated a new point-of-care tool that clinicians can use to objectively quantify and longitudinally track outcomes in patients with benign and malignant esophageal conditions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Development and validation of the Cleveland Clinic Esophageal Questionnaire (CEQ) were recently described in the Journal of Thoracic and Cardiovascular Surgery [Epub 23 Aug 2023], and now a study presented at the American College of Surgeons Clinical Congress 2023 shows that the CEQ detects important differences in eating and dyspepsia in achalasia patients that are not captured by the Eckardt symptom score (ESS). The study also demonstrated utility of the CEQ’s novel “bother” T-score aimed at determining the impact of symptoms on a patient’s quality of life.
“Our research shows that the CEQ provides a better objective quality-of-life assessment in achalasia patients than the Eckardt symptom score,” says thoracic surgeon Monisha Sudarshan, MD, principal investigator of the study. “It takes under five minutes to complete and can be used to reliably surveil patients with a wide variety of esophageal conditions.”
Written at a third-grade level, the CEQ is the only validated patient-reported outcome measure applicable to all esophageal diseases. It was developed beginning in 2020 based on an extensive literature review, expert opinion and previously unpublished Cleveland Clinic research. A pilot version of the questionnaire was tested at Cleveland Clinic’s thoracic surgery outpatient clinic, after which it was further refined based on patient feedback.
The final 34-item instrument spans six domains:
Advertisement
Patients are asked to rate each symptom on a frequency scale from “never” to “several times a day” and to rate the “bother” caused by each symptom on a scale from “not at all” to “a lot.” The figure below presents a sample portion of the CEQ and bother questionnaire.
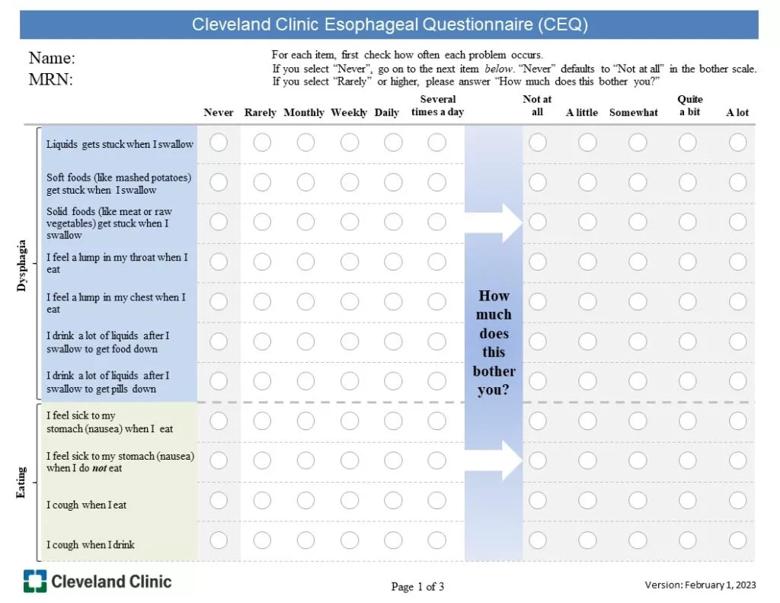
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/23f5ee74-8e2c-405e-b508-55e9ec5dd17f/Slide1-1024x791_jpg)
Figure. A sample portion of the Cleveland Clinic Esophageal Questionnaire (CEQ).
In contrast, the gold-standard ESS is written at a higher reading level (dependent on the clinician administering it), grades the frequency of only four symptoms (dysphagia, regurgitation, chest pain and weight loss) and has no “bother” component.
“It was particularly important to us to measure bother because the impact of a symptom can vary from patient to patient,” Dr. Sudarshan says. “Mild dysphagia, for example, may be very troubling to some individuals, whereas even significant dysphagia is not a problem for other patients.”
According to Sadia Tasnim, MD, a Cleveland Clinic thoracic surgery research fellow and study co-author, the researchers also believed the CEQ should measure the ability to eat. “Ability to eat is a better assessment of achalasia symptoms than weight loss because weight loss can be influenced by several other confounding factors,” she explains.
For the new study presented at the American College of Surgeons meeting, use of the CEQ and the ESS was compared in 28 English-speaking adults with achalasia scheduled to undergo either Heller myotomy with Dor fundoplication or per oral endoscopic myotomy (POEM). Patients had a mean age of 59 years and were predominantly female (57%) and white (93%). The two questionnaires were administered to the cohort before and approximately three months after their respective procedures, which were performed from January 2022 through January 2023.
Advertisement
Differences in pre- and post-surgery scores were calculated using a paired t-test, with effect size measured using Cohen’s d (0.2 = small effect, 0.5 = medium, 0.8 = large).
On the three symptom domains that are common to all three scores — dysphagia, pain and reflux/regurgitation — the CEQ, its bother T-score and the ESS all detected statistically significant large effect size differences between the pre- and post-surgery time points (Cohen’s d range, 0.88-2.59; P < 0.001).
Additionally, the CEQ and the bother T-score detected statistically significant effect size differences before and after surgery in the eating and dyspepsia domains (Cohen’s d range, 0.76-1.19; P < 0.001).
“The CEQ was comparable for the same domains measured by the Eckardt symptom score,” says Dr. Tasnim, “and we were surprised that it also documented significant improvements in dyspepsia post-surgery, which is not part of the Eckardt score.”
As reported in the recent Journal of Thoracic and Cardiovascular Surgery paper, validation of the CEQ was performed in a cohort of 546 patients (mean age, 62 years; 53% male, 86% white), more than 90% of whom completed it within five minutes. Construct validity was demonstrated by differentiating scores across conditions including esophageal cancer, achalasia, hiatal hernia and other diagnoses.
To date, the CEQ has been used in the care of more than 1,100 patients with esophageal complaints at Cleveland Clinic. The next steps are to incorporate the questionnaire into the institution’s electronic medical record and to seek multi-institutional validation of the instrument.
Advertisement
“Every patient with an esophageal disease who walks through our clinic’s doors is completing this questionnaire, and we intend to administer it at every visit so we can amass longitudinal data,” Dr. Sudarshan notes. “We are also working to extend use of the CEQ to other departments that see patients with esophageal disease and to surgeons in our local Veterans Affairs hospital.”
Advertisement
Advertisement

25-year series of over 1,000 patients reveals good long-term palliation, esophageal preservation

Case highlights the benefits of a minimally invasive approach

3 pediatric gastroenterologists discuss advances in their diagnostic toolkits

Modified Barium Swallow Study and Flexible Endoscopic Evaluation of Swallowing can both be used to diagnose dysphagia, but it’s important to understand their advantages and disadvantages

Microvascular “supercharging” is a critical newer step to promote favorable outcomes

Research could help direct care pathways for patients with unexplained swallowing difficulties

Potential for new, non-invasive screening option

Pediatric and adult gastroenterologists offer team care for patients with eosinophilic esophagitis