Parenchymal volume analysis is more accurate and more convenient
Partial nephrectomy or radical nephrectomy? That’s one of the biggest decisions clinicians need to make for patients who have localized kidney cancer. Partial nephrectomy preserves more kidney function, but radical nephrectomy is often the stronger choice oncologically, at least for patients with larger tumors or those with potentially aggressive findings on imaging, says Steven C. Campbell, MD, PhD, of the Center for Urologic Oncology at Cleveland Clinic’s Glickman Urological & Kidney Institute.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To help make the best choice, urologic surgeons often estimate glomerular filtration rate (GFR) of the contralateral kidney (without the tumor) by calculating split renal function. Conventionally that’s been done by a nuclear renal scan — a test that shows relative kidney activity based on filtration of a radioactive isotope.
“The problem with nuclear renal scans is multifold,” says Dr. Campbell. “First, it’s an extra test that the patient needs to undergo. There’s some added cost involved. There’s some radioisotope exposure, albeit very small. And nuclear renal scans are notorious for their inaccuracy.”
That’s why the kidney transplant world — which also relies on split renal function to determine which kidney to remove from a living donor — no longer uses nuclear renal scans. Instead they ask radiologists to use computerized software to perform parenchymal volume analysis based on a potential donor’s CT or MRI scan. Nephron mass correlates extremely well with function, says Dr. Campbell. And it requires no additional procedure, given that most patients have already had cross-sectional imaging.
“I went to AUA in 2019 and was talking to transplant colleagues about our hypothesis that parenchymal volume analysis could work for kidney cancer patients too,” says Dr. Campbell. “I knew that kidney cancer patients wouldn’t be as ‘clean’ as the relatively young and healthy kidney donor population, but it was still worth a try.”
Turns out he was right. Results of a retrospective study of 529 patients with renal tumors managed at Cleveland Clinic from 2010 to 2018 were recently published in BJU International. It’s the first publication to convincingly show the utility of parenchymal volume analysis in kidney cancer, says Dr. Campbell.
Advertisement
How would this be useful in routine clinical practice? Dr. Campbell poses this example: A patient has a somewhat large, potentially aggressive tumor in the right kidney, and the tumor is somewhat centrally located. Radical nephrectomy is thus a strong consideration for oncologic reasons.
The preoperative global GFR is 72. Previous studies have shown that if the new baseline GFR after renal cancer surgery is greater than 45, patients tend to have survival characteristics similar to patients who do not have chronic kidney disease.
Average degree of renal functional compensation after a radical nephrectomy is 20-25%. In a patient like this, the split renal function will often be about 55% in the contralateral kidney, due to some degree of parenchymal volume replacement by the tumor. In this case, the contralateral kidney would have a baseline GFR of 72 x 0.55, or about 40. With renal functional compensation, the new baseline GFR after radical nephrectomy would be about 48-50. Hence, radical nephrectomy may be a very reasonable option in this patient, particularly if partial nephrectomy would be challenging and associated with some degree of perioperative or oncologic risk.
“I would feel comfortable recommending radical nephrectomy for this patient because their new baseline GFR will be above 45,” says Dr. Campbell. “Of course, if the patient is relatively young or has other comorbidities that can affect renal function, or if there is a concern about familial kidney cancer, that would change the equation. Outside of such special considerations, radical nephrectomy would be a strong consideration in such a patient.”
Advertisement
“What we didn’t know going into our study was the reliability of parenchymal volume analysis in an older population of patients with diabetes and other comorbidities, which commonly defines people with kidney tumors,” says Dr. Campbell.
The team of researchers compared estimated filtration rates in a cohort of 374 partial nephrectomy patients and 155 radical nephrectomy patients as determined by split renal function from parenchymal volume analysis and split renal function from nuclear renal scan.
“Not only did we show that split renal function from parenchymal volume analysis correlated with split renal function from nuclear renal scan, we showed that it was more accurate, even for these complex patients,” says Dr. Campbell. “For this, we looked at the relationship between parenchymal volume saved and function saved in the operated kidney in patients managed with partial nephrectomy with cold ischemia. Previous studies had shown a strong correlation between these factors (mass saved = function saved). For these analyses, split renal function is required to calculate the function in the operated kidney before and after surgery. When split renal function was derived from nuclear renal scans, the r factor for correlation between mass saved and function saved was only 0.62, which is good but not great. When split renal function was derived from nuclear renal scans, the r factor for the correlation was 0.74, which is much more impressive. This was a statistically significant difference in r factors. This suggests that split renal function from nuclear renal scans was introducing some element of variability or error in measurement that was not seen with parenchymal volume analysis.”
Advertisement
With these convincing findings, Dr. Campbell argues that it’s time to replace nuclear renal scans with parenchymal volume analysis for patients with kidney tumors. Not only is it more accurate, it costs less than ordering a nuclear renal scan and uses technology that radiology has already been using for kidney transplant donors. The software to calculate parenchymal volumes with exclusion of the tumor is very easy to use, says Dr. Campbell, and the calculation only takes a few minutes.
Dr. Campbell has begun using parenchymal volume analysis in his routine clinical practice. While not necessary for patients with small tumors needing only a partial nephrectomy, it’s applicable for about 20-30% of the patients he sees, those with larger and more aggressive-looking tumors.
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

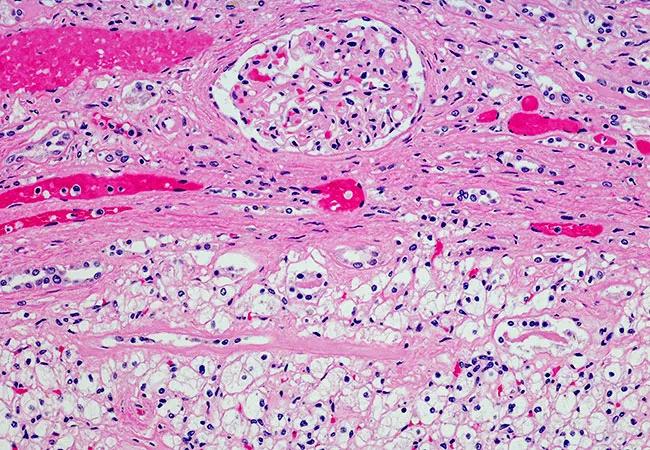
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key