Careful diagnosis, stepwise management can improve symptoms
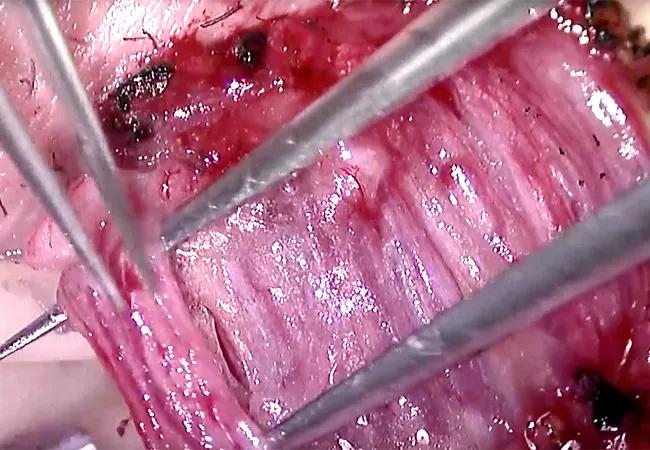
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b784dc75-a819-47dc-bc0d-ca28fb439c11/17-URL-929-Orchialgia-Shoskes_jpg)
17-URL-929 Orchialgia Shoskes
By Daniel Shoskes, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Orchialgia, also known as chronic testicular pain or chronic scrotal contents pain, is a condition that has long been a neglected diagnosis in urology.
Unlike most urologic men’s health conditions, we have limited data on incidence (although every practicing urologist who sees men knows that it’s common), no information on natural history, no validated symptom score/outcome measure, and no randomized controlled trials of medical therapy.
While data is sparse, we do know that a clear, stepwise approach to diagnosis and therapy can lead to improvement in many men.
Orchialgia may develop on its own or following infection, trauma, inflammation or surgery (e.g., vasectomy, hernia repair) or due to a hydrocele. Pain can also be referred to the scrotum from another source (e.g., a ureteral stone).
Clearly, any known reversible testicular cause should be diagnosed and treated. Pain due to pelvic floor muscle spasms is not difficult to appreciate on physical exam and can be treated with pelvic floor physical therapy. Other conservative measures are best to try for at least three months. These include rest, heat, tight-fitting underwear, oral anti-inflammatory medications (e.g., ibuprofen) and medications for neuropathic pain (e.g., gabapentin, pregabalin).
If pain persists, an important diagnostic test is injection of a local anesthetic into the spermatic cord at the level of the pubic tubercle. This cord block should anesthetize the genital branch of the genitofemoral nerve and inguinal branches of the ilioinguinal nerve. If the cord block doesn’t eliminate the pain, referral to a pain management physician may be warranted. Unfortunately, there is little outcome data regarding orchialgia treatment with chronic pain management approaches.
Advertisement
Microscopic spermatic cord denervation (MSCD). If the cord block is successful, eliminating the pain temporarily, we recommend MSCD performed through a subinguinal incision. In this outpatient surgery, the cord is exposed and using an operating microscope and meticulous microsurgical technique, the blood and lymphatic supply of the testicle are preserved and remaining structures, which contain the nerves, are transected. If a cord block was successful, the surgery provides durable cure of the pain in 75-80 percent of cases.
Microscopic vasovasostomy. An alternative for men with postvasectomy pain is microscopic vasovasostomy. While its published outcomes are similar to MSCD postvasectomy, vasovasostomy does restore fertility and may only address pain in the subset of men who have congestive back pressure on the epididymis rather than neuropathic pain as their underlying pathophysiology.
At the Cleveland Clinic, our experience with MSCD is durable elimination of pain in slightly over 80 percent of patients. In the 20 percent who did not improve, several patients admitted that the cord block may not have eliminated their pain and several had pelvic floor spasm identified but declined doing physical therapy. Nevertheless, morbidity has been minimal with one hydrocele and one orchiectomy for persistent pain with poor arterial flow in the past 65 cases.
Levine LA, Hoeh MP. Evaluation and management of chronic scrotal content pain.
Curr Urol Rep. 2015 Jun;16(6):36.
Larsen SM, Benson JS, Levine LA. Microdenervation of the spermatic cord for chronic scrotal content pain: single institution review analyzing success rate after prior attempts at surgical correction. J Urol. 2013 Feb;189(2):554-8.
Advertisement
Benson JS, Abern MR, Larsen S, Levine LA. Does a positive response to spermatic cord block predict response to microdenervation of the spermatic cord for chronic scrotal content pain? J Sex Med. 2013 Mar;10(3):876-82.
Advertisement
Advertisement
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
Oncologic and functional outcomes are promising, but selection is key