Cardiothoracic surgeon José Luis Navia, MD, Florida Regional Director of the Heart, Vascular, and Thoracic Institute for Cleveland Clinic, performed the first robotic-assisted mitral valve repair at Cleveland Clinic Weston Hospital in January 2022, launching southeast Florida’s only Robotic-Assisted Mitral Valve Surgery Program and joining just over 100 centers in the United States to offer this surgical approach.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The program is now on track to achieve a program milestone, performing 20 robotic-assisted valve repairs in its first year. “Patient preference for less invasive surgery that offers a quicker recovery is driving the momentum we’ve seen in our program’s inaugural year,” says Dr. Navia.
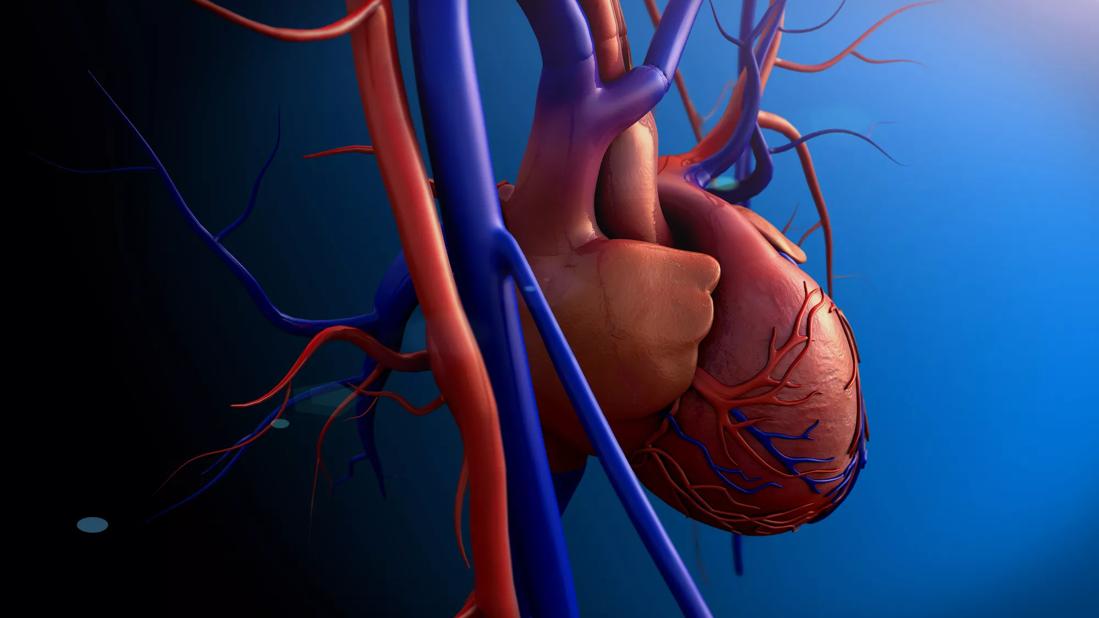
According to the American Heart Association, about 2% of the U.S. population has mitral valve prolapse (MVP), when one or both flaps partially collapse into the left atrium allowing the backward flow of blood to occur. While few will experience problems associated with the condition, serious MVP cases can cause life-threatening complications like arrhythmias and heart failure.
Joe Santoro, 57, is a textbook example of MVP, the most common cause of chronic primary mitral regurgitation. He lived with mitral valve disease for almost a decade before developing shortness of breath, fatigue and activity decline, classic symptoms of disease progression that included the onset of atrial fibrillation (AF). At that point, Santoro’s cardiologist advised him to undergo a heart valve procedure.
The first-grade teacher and musician sought a second opinion at Cleveland Clinic Florida, where Dr. Navia confirmed it was time to surgically repair the bileaflet mitral valve prolapse and associated AF. “Ideally, I would like to have treated Joe before his valve prolapse impacted the function of his left atrium, because we know surgery is most effective when symptoms have not advanced too far,” says Dr. Navia.
The American College of Cardiology and American Heart Association issued updated Practice Guidelines for Management of Patients with Valvular Heart Disease in 2020 that recommend early surgery for patients with degenerative mitral valve disease if there is a high chance of successful repair and mortality risk is low. But according to Dr. Navia, he is still seeing many patients with mitral valve disease, like Santoro, who have reached a chronic stage prior to referral for surgery.
Advertisement
Following comprehensive diagnostic testing that included a transesophageal echocardiogram, chest x-ray, and CT angiogram, it was determined that Santoro was eligible for all three major surgical approaches for valve surgery now offered at Cleveland Clinic Weston Hospital – robotic, minimally invasive, and open.
Traditional open-chested mitral valve surgery involves creating a 6- to 8-inch incision through the sternum and spreading the ribs to view the heart. Minimally invasive surgery with handheld instruments requires a 3 to 4 inch incision and may be performed with or without rib-spreading.
The robotically-assisted technique uses even smaller incisions, often less than 2 inches. With the robotic arms deployed in the right thorax, the procedure typically entails peripheral perfusion and aortic occlusion.
“Because of Joe’s age, lack of comorbidities, and ejection fraction he was a candidate for robotic-assisted surgery,” says Dr. Navia, noting the approach is usually recommended for younger patients like Santoro. “He had none of the contraindications for this approach, which include aortic insufficiency, severe pulmonary hypertension, annular calcification, and poor ventricular function.”
Santoro chose the least invasive option because he would heal faster and be able to return to his normal activities more quickly. Other benefits included lower risk of infection, less bleeding and trauma, a shorter hospital stay, and better cosmesis.
Dr. Navia used the robotic-assisted approach to address the valve prolapse, performing a posterior and anterior leaflet repair and annuloplasty. Concomitant procedures also were performed to address the atrial fibrillation, including closure of the left atrial appendage and cryoablation.
Advertisement
Three weeks after major heart valve surgery, Santoro was back to performing with his band. “I was jumping around, playing guitar and singing. I felt perfectly fine. It was amazing,” he says.
According to Dr. Navia, almost all of the patients he’s consulted with who met the criteria chose robotic-assisted valve surgery. “Only two patients, both women with breast implants, were not found to be eligible for the robotic approach,” he adds.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.