Cleveland Clinic screening tool yields results comparable to those with sternotomy

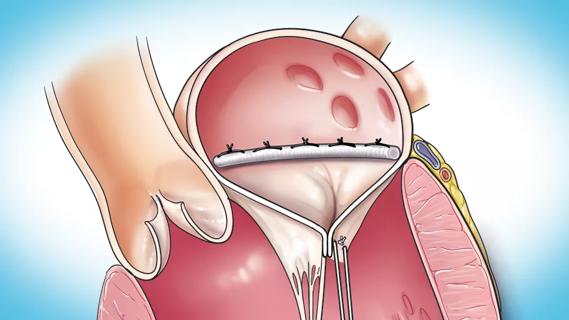
An algorithm for selecting patients with isolated degenerative mitral valve disease for robotically assisted surgery can lead to outcomes similar to those for patients undergoing sternotomy, with some additional benefits. So finds a nonrandomized study of the Cleveland Clinic-developed algorithm, which bases patient selection on transthoracic echocardiographic and CT features. The study and the algorithm itself were published in the Journal of Thoracic and Cardiovascular Surgery (2022;164[4]:1080-1087).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our algorithm led to 60% of patients with isolated degenerative mitral valve disease qualifying for robotic surgery across a 1,000-patient sample,” says the study’s senior author, Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic. “Postoperative outcomes were excellent and comparable to those of patients undergoing mitral valve surgery with sternotomy, which validates this screening approach.”
Although robotic surgery is the least invasive surgical option for mitral valve repair, it is used in only a small percentage of cases nationwide. Concerns persist despite studies indicating that its safety and effectiveness are comparable to those with sternotomy. In addition, the robotic approach confers several benefits common to minimally invasive operations, including fewer complications, shorter hospital stay and better cosmetic results.
The algorithm requires that candidates for robotic mitral valve surgery fulfill the following requirements based on imaging findings:
From transthoracic echocardiography:
From CT of the chest, abdomen and pelvis:
The algorithm also excludes patients with absolute contraindications to robotic mitral valve surgery, including previous thoracotomy, extensive calcification of the aortic root or ascending aorta, severe pulmonary dysfunction and severe liver dysfunction.
Advertisement
During a five-year period from 2014 to 2019, the screening algorithm was rigorously applied by three Cleveland Clinic surgeons to determine candidacy for robotic surgery among 1,000 consecutive patients scheduled for surgery for isolated degenerative mitral valve regurgitation. Under the algorithm, 605 patients were selected for robotic surgery (60.5%) and 395 for sternotomy (39.5%).
The most common reasons for disqualifying a patient for robotic surgery were as follows (42% of patients had multiple disqualifying criteria):
Patients undergoing the robotic approach were younger (mean age of 56 ± 10 vs. 60 ± 12 years) and more likely to be male. They also had a slightly greater mean ejection fraction, a better mean New York Heart Association functional class and fewer baseline comorbidities.
All patients underwent mitral valve repair except for four in the sternotomy group, who underwent valve replacement. Valve repair led to no or only mild mitral regurgitation in 99.7% of patients at discharge. No operations involved conversion from robotic surgery to sternotomy.
No hospital deaths occurred across the cohort, and rates of postoperative stroke were similar between the groups (0.5% in the robotic group vs. 1.0% in the sternotomy group).
Patients who underwent robotic surgery had several benefits compared with sternotomy patients, including:
Advertisement
Dr. Gillinov emphasizes that preoperative CT of the chest, abdomen and pelvis is important for ensuring safe and effective femoral perfusion.
“After instituting routine CT scanning for patients undergoing robotic surgery, we cut our stroke rate by more than half,” he notes. “For borderline vessels, we expose the femoral vessels before chest incision and port placement. In rare cases, we may switch to sternotomy on that basis.”
The study authors emphasize that the Cleveland Clinic algorithm, which stemmed from their needs during their initial experience with robotic mitral valve surgery, is just one approach for determining candidacy for the procedure. “This is not meant to be prescriptive for others or to hinder further application of robotic mitral valve surgery,” Dr. Gillinov says.
He adds that since his team has grown its experience, they have extended robotic surgery to patients with some degree of left ventricular dysfunction, mild mitral annular calcification and the need for concomitant procedures.
Despite the lack of a prescriptive intent behind the algorithm, a commentary accompanying the study notes that a conservative screening strategy of this type may be particularly relevant in centers that are starting a robotic mitral valve surgery program.
Advertisement
Advertisement

NIH-funded comparative trial will complete enrollment soon

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Two surgeons share insights on weighing considerations across the lifespan

An overview of growth in robot-assisted surgery, impressive re-repair success rates and more

Judicious application yields a 99.7% repair rate and 0.04% mortality
Cleveland Clinic series supports re-repair as a favored option regardless of failure timing

A call for surgical guidelines to adopt sex-specific thresholds of LV size and function