Study validates a noninvasive alternative to invasive coronary angiography
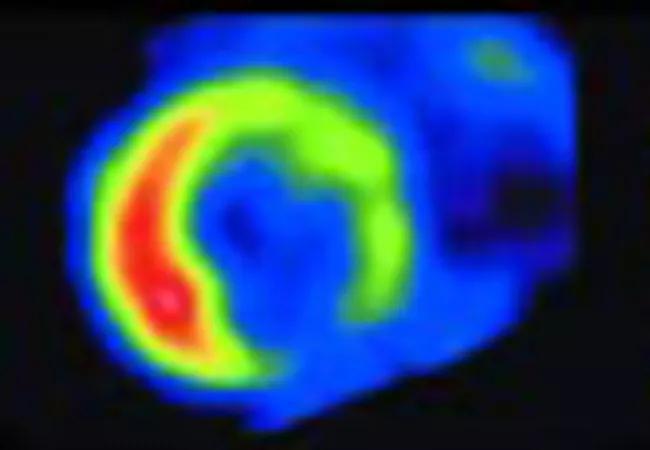
Positron emission tomography/computed tomography (PET/CT) scanning with myocardial blood flow (MBF) quantification has high diagnostic and prognostic accuracy for cardiac allograft vasculopathy (CAV), making it a reasonable noninvasive alternative to invasive coronary angiography (ICA) to screen for this often-fatal complication in heart transplant patients.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So concluded a team of Cleveland Clinic cardiologists who assessed a previously published algorithm based on PET with MBF, using a larger population than was used to develop the algorithm as well as a more readily available tracer, rubidium (Rb-82). The study was published in JACC Heart Failure (2023;11:555-565).
“Based on experience with more than 400 patients, we found that PET/CT scanning with MBF performs well for ruling in or out moderate-to-severe CAV,” says the study’s senior author, Wael Jaber, MD, a Cleveland Clinic cardiologist. “It thus offers a reasonable option for screening heart transplant patients for CAV that entails less risk than current practice.”
CAV typically develops asymptomatically or with atypical symptoms, necessitating periodic surveillance after heart transplantation. Standard of care involves screening with ICA, with or without intravascular ultrasonography. “This involves high expense and risks inherent in the invasive procedure, as well as frequent exposure to iodinated contrast,” says heart failure cardiologist Randall Starling, MD, MPH, a study co-author. “This prompted a search for better options.”
PET/CT with MBF was proposed as a possible alternative to ICA, and Bravo and colleagues developed a promising algorithm based on 66 patients, using 13N-ammonia as the PET tracer and a mixture of regadenoson and adenosine as vasodilator stress agents. The current study was designed to validate this algorithm on a larger patient population and explore use of the more widely available Rb-82 as the tracer and only regadenoson as the stress agent.
Advertisement
Patients who underwent heart transplantation at Cleveland Clinic and had PET scans (using a hybrid PET/CT scanner) with MBF quantification between 2015 and 2021 were retrospectively assessed. The following two major areas were evaluated:
The proposed algorithm classified the 401 patients as follows:
Key results regarding diagnostic accuracy were as follows:
Regarding prognostic value of the proposed algorithm:
Advertisement
The results indicate that the algorithm has the ability to rule in or rule out significant CAV with high certainty, and it appropriately stratifies the short-term risk of the need for revascularization, the authors note.
“Confirming the original findings during development of the algorithm with a larger validation cohort and using the more widely available Rb-82 as a stress agent increases the applicability of this approach,” says Dr. Jaber. “We can conclude that PET/CT scanning with MBF is a reasonable method for CAV screening.”
“By enabling evaluation of multiple measures, including myocardial perfusion imaging, myocardial blood flow and myocardial flow reserve, PET offers robust noninvasive assessment of the microcirculation as well as epicardial manifestations of CAV,” adds the study’s first author, Cleveland Clinic cardiovascular medicine fellow Bryan Abadie, MD.
The authors add that future studies are needed using larger populations and longer follow-up, and they call for the creation of multicenter registries with serial PET images of patients with heart transplants. In addition, the best timing of screening initiation after heart transplantation has yet to be determined, as does the optimal surveillance interval between PET scans.
Advertisement
Advertisement

Largest study to date confirms mortality rates similar to DBD transplant and reveals risk factors

More than 30% of patients die when early dialysis is needed after surgery

Highlights and insights from recent Cleveland Clinic experience

Results from a large registry study provide an updated picture of recurrent rejection

Findings from more than 7,500 donor-recipient pairs

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more

Milestone minimally invasive surgeries reduce pain and recovery time