Few patients report left ventricular dysfunction or heart failure after one year
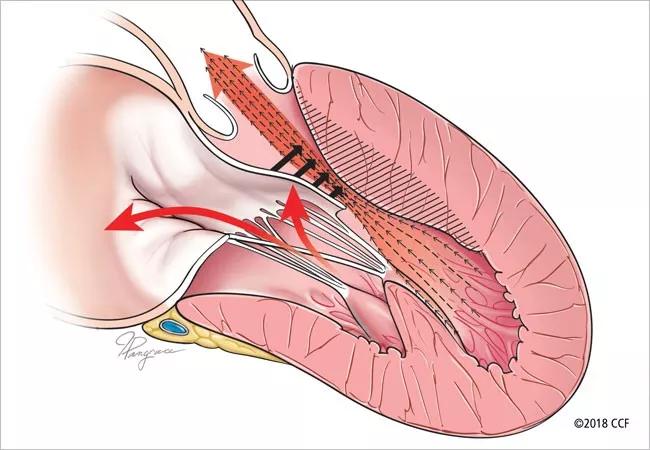
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/73c795b4-665a-47ef-9631-4732ff4f8326/22-HVI-3509429_obstructive-hypertrophic-cardiomyopathy_650x450_jpg)
Obstructive hypertrophic cardiomyopathy
Mavacamten continues to show favorable real-world results in patients with obstructive hypertrophic cardiomyopathy (HCM), according to a new analysis of more than 6,000 patients receiving the drug through the FDA’s Risk Evaluation and Mitigation Strategy (REMS) program. Few patients were reported to have left ventricular dysfunction or heart failure after one year of taking the drug.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Study results were presented at the 2024 American Heart Association Scientific Sessions by the study’s lead author, Milind Desai, MD, MBA, Director of the Hypertrophic Cardiomyopathy Center at Cleveland Clinic. Results also were published in Circulation: Heart Failure.
These results echo the favorable findings from an earlier study of the first 150 Cleveland Clinic patients to receive mavacamten through the REMS program.
“Not only did our newest study report efficacy in a much larger U.S. population over a longer period of time — the first 22 months of mavacamten’s availability in the U.S. — we found that most patients were treated sufficiently with only 5 or 10 mg per day,” says Dr. Desai, who was principal investigator for the pivotal VALOR-HCM trial that supported mavacamten’s FDA approval in 2022. “These findings add to the growing evidence that mavacamten is effective in providing a better quality of life for patients with HCM, delaying or preventing their need for septal reduction therapy.”
A novel cardiac myosin inhibitor, mavacamten is the first drug in the U.S. to be approved for the treatment of symptomatic obstructive HCM. Phase 3 clinical trials indicated that the drug improved patients’ left ventricular outflow tract (LVOT) gradient, symptoms and physical function, as well as reduced their need for septal reduction therapy (SRT).
However, the drug also reduces left ventricular ejection fraction (LVEF), which can lead to heart failure. As such, mavacamten is currently available only through the REMS program, an FDA effort to ensure safe use. The program requires monitoring patients for heart failure and LVEF below 50%, as assessed through regular echocardiograms. It also requires regular screening for drug interactions.
Advertisement
“Mavacamten offers a new option for patients with obstructive HCM, whose symptoms and quality of life are not improved with beta blockers, calcium channel blockers or disopyramide, and who may not have easy access to a tertiary center that performs SRT,” Dr. Desai says.
According to records in the REMS database, 6,299 patients were treated with one or more doses of mavacamten from April 2022 through February 2024. Of these patients, 60% were women and 65% were older than age 60.
Patient status forms were submitted for 5,573 patients. Of those patients:
Those percentages were comparable or even lower for the 1,929 patients who were treated with mavacamten for one year or longer:
Other key findings involved:
Advertisement
“This is the largest study to date on mavacamten, so we were pleased that so few patients taking the drug recorded LVEF under 50% or heart failure symptoms requiring hospitalization,” Dr. Desai says. “Very few needed to stop taking mavacamten as a result, and those who did eventually resumed treatment. This is very encouraging.”
In addition to tracking these favorable outcomes, the REMS program appears to be effective in monitoring patient safety. Prescribers and pharmacies complied with the program, dispensing mavacamten only when appropriate, according to echocardiograms and other assessments recorded on REMS patient status forms. Very few patients received contraindicated medications, and few required a lower dose of mavacamten due to drug-drug interaction.
Future studies are needed to determine if the number and frequency of echocardiograms could be decreased.
“It is good to see that the broader, real-world experience in the mavacamten REMS program is comparable to the trial data for the medication, as well as our own experience at Cleveland Clinic,” adds Maran Thamilarasan, MD, a Cleveland Clinic cardiologist who was not involved in the study. “We eagerly await data on the potential longer-term effects and benefits of this medication.”
The study was funded by Bristol Myers Squibb, parent company of MyoKardia, the developer of mavacamten. Dr. Desai reports that he is a consultant for Bristol Myers Squibb.
Advertisement
Advertisement
End-of-treatment VALOR-HCM analyses reassure on use in women, suggest disease-modifying potential
Cardiac imaging substudy is the latest paper originating from the VANISH trial
Vigilance for symptom emergence matters, a large 20-year analysis reveals
Phase 3 ODYSSEY-HCM trial of mavacamten leaves lingering questions about potential broader use
5% of flagged ECGs in real-world study were from patients with previously undiagnosed HCM
High composite score in myectomy specimens signals worse prognosis
Avoidance of septal reduction therapy continues while LVEF dysfunction remains infrequent
New risk score pools factors that may predict adverse outcomes in the uncommon phenotype