Latest concepts in the surgical creation of functional, opposable thumbs in early childhood

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e8950971-ba26-4183-b858-103d831248d4/22-ORI-3183860-CQD-650x450-1_jpg)
22-ORI-3183860 CQD 650×450
By Joseph Styron, MD, PhD, and William H. Seitz Jr., MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are a multiplicity of congenital conditions resulting in hypoplasia or absence of a child’s thumb. These include:
Each of these conditions provides a challenge for developing thumb opposition and, therefore, functional prehension in the developing child. At Cleveland Clinic, decades of experience in managing the spectrum of these conditions have enabled us to develop multiple techniques to achieve prehensile hand function in patients requiring an opposable thumb or a thumb positioned in opposition to which other fingers can converge to grasp and pinch.1-5
In all cases, the goal for opposed prehension is positioning a thumb pronated 90 degrees from the broad plane of the hand, palmarly abducted 45 degrees from the hand, and able to cross the midline of the palm with a wide and adequately deep first webspace. From this position, even a thumb acting as a rigid post can provide a very precise and sensate tip pinch and chuck pinch by bringing the ulnar digits to its distal end.1,2,6-9
Ideally, however, the ability of the thumb to flex, extend, abduct and actively oppose can be achieved in many cases. Our experience has enabled us to develop techniques for reconstruction of thumbs previously believed to be unreconstructible. In those that are truly unreconstructible, we can convert a healthy index finger into a mobile, opposable, functional thumb through refinement of prior techniques of pollicization.4,10-16
Advertisement
Determining the need for reconstruction versus pollicization is based partly on the modified Blauth classification system of congenital thumb hypoplasia.1,2,7,9,16-17
Advertisement
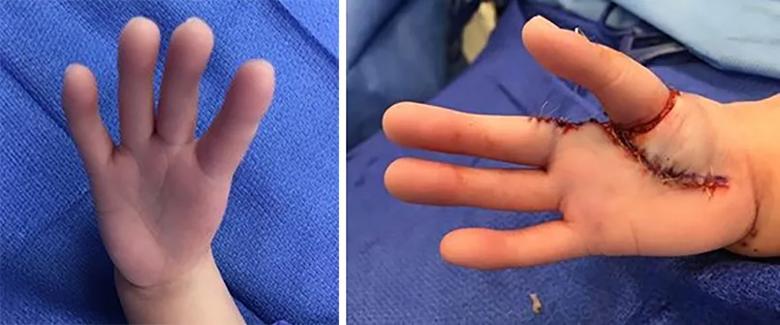
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4a50e8ed-7bd4-4226-803a-a655de82d661/22-ORI-3183860-CQD-inset-combo_jpg)
Figure 1. Before and after pollicization to treat type V hypoplastic thumb.
Accepted surgical practice presumes that any attempt to reconstruct a type III hypoplastic thumb will be unsuccessful. As such, it has become the convention to amputate type III thumbs and proceed with pollicization, typically using the index finger.
Pollicization does have the advantage of being a single-stage surgery, although some cases require secondary opponensplasty. It offers a relatively fast and simple recovery by preserving the neurovascular bundles and tendons of the index finger as it becomes a thumb.
Nevertheless, it can be difficult for parents to choose pollicization, essentially prioritizing function over form. Amputating the hypoplastic thumb and performing a pollicization means the child will not have all 10 digits. Parents often seek a functional alternative. Therefore, we always present reconstruction and pollicization options during our consultations.
Doing nothing is a third option. However, children who do not have treatment for their nonfunctional hypoplastic thumb often resort to scissor pinching between the index and middle fingers. This scissor pinch is much more noticeable as a behavioral difference than a pollicization or reconstruction that allows the child to grasp and manipulate objects more naturally, as people do not routinely count fingers outside of a newborn nursery.
Creation of a functional, mobile, stable opposable thumb requires appropriate skeletal substance and support; stable carpometacarpal (CMC) and MP joints; flexion, extension, abduction and opposition motors; appropriate thumb positioning; and an adequately wide and deep first webspace.
Advertisement
In types I and II conditions, this will require stabilization of the MP joint through augmentation of the ulnar collateral ligament with suture imbrication of the capsule and either an abductor digiti minimi (ADM) (Huber) or flexor digitorum superficialis (FDS) opponensplasty through an ulnar sling. In these cases, usually there is an existing extrinsic flexor and extensor.19-21
Type III conditions usually require transfer of bone. At Cleveland Clinic, we have been highly successful in transferring one or two autologous second-toe proximal phalanges, harvested extraperiosteally, to create a metacarpal as well as a carpal receptacle/capsular pouch to create a CMC joint. The joint is sutured around the base of the most proximal transferred toe phalanx. This has been performed with minimal to no complication at the donor site. All physeal plates are preserved with their periosteal sheath. At the same time, a Z-plasty widening and deepening of the first webspace is performed to position the new thumb anatomically. Through the Z-plasty incision, a capsulorrhaphy/collateral ligament imbrication is performed.2,4,5,18
These reconstructions are held with one or two fine K-wires and appropriate thumb position in a long arm cast for six weeks. At that point, the cast and K-wires are removed in office, and a soft splint is fabricated from foam material and used for support for another month.
Six months after the initial surgery, secondary surgery is performed, which generally includes Huber opponensplasty, transfer of the ring superficialis flexor tendon for flexor pollicis longus function, and transfer of extensor indicis proprius tendon for extensor pollicis longus function (Figure 2).1,2,6,9
Advertisement
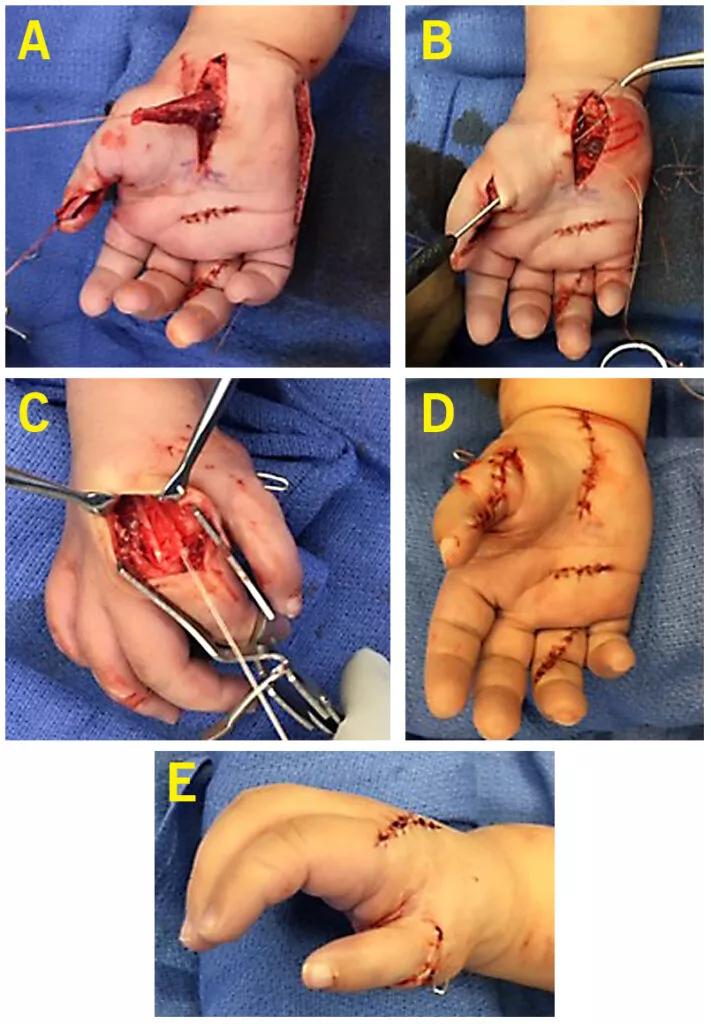
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1027b1f6-3750-46f5-b363-f5dadf74cfce/22-ORI-3183860-CQD-inset-711x1024_jpg)
Figure 2. ADM muscle has been mobilized from the ulnar side of the hand and passed through subcutaneous tissue in preparation for passing it to the radial side of the hand and thumb MP joint (A). FDS of the ring finger has been released from its attachment and passed through the carpal canal and along the surface of the transplanted toe phalanges to the interphalangeal joint of the thumb for attachment as a flexor pollicis longus (B). The extensor indicis proprius is mobilized from the back of the hand and passed radially in the path of a normal extensor pollicis longus tendon and secured to allow both extension and abduction of the thumb (C). Final posture of the hand with transferred tendons and muscle (D,E).
In rare cases, we have found limited growth of the transferred toe phalanges and performed distraction lengthening of the transferred bone.3,5,10-15,22,23 However, with current surgical techniques, this procedure is typically not needed.
Again, the new thumb is held in position with K-wires and a long arm cast for six weeks, followed by one month in a foam splint. At that point, the child is encouraged to start using the hand and thumb independently. Long-term follow-up has demonstrated remarkable functional outcomes in these patients, with continued growth, as seen in this video of a patient following reconstruction.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/700aEIYiXdU?feature=oembed)
Outcome of thumb hypoplasia reconstruction (Child #1)
Although pollicization has been accepted as a treatment of choice for most forms of thumb hypoplasia, it certainly is a reasonable option for patients with types IV and V conditions, where there is not an adequate skin bridge or the thumb is completely absent.
The presence of a stable CMC joint is also a determining factor. A hypoplastic thumb without a stable CMC joint is better treated with pollicization versus reconstruction. In addition to the technical skill of the surgeon, the success of the pollicized digit depends on whether the index finger is supple, and whether the thumb hypoplasia is in isolation or part of an absent radius.
Again, the principle for thumb reconstruction is to have a thumb adequately positioned at 45 degrees of abduction away from the palm, with 90 degrees of pronation and ability to oppose across the midline. A number of techniques have been developed by pioneers including Buck-Gramcko, Carroll, Ezaki, Upton and Manske, all building on each other’s experiences.7,8,16
At Cleveland Clinic, we have used combinations of these techniques to best position the new thumb; provide healthy, minimally scarred first webspace through broad full-thickness flaps of skin and subcutaneous tissue; and shorten the metacarpal with ablation of the physeal plate at the neck of the metacarpal to prevent overgrowth. The metacarpal head acts as a trapezium, allowing the three phalanges of the index finger to replicate the metacarpal and two phalanges of the thumb. Advancement and tensioning of flexor tendons of the index and its extensor tendons provide the needed flexion, extension, opposition and abduction (Figure 3).
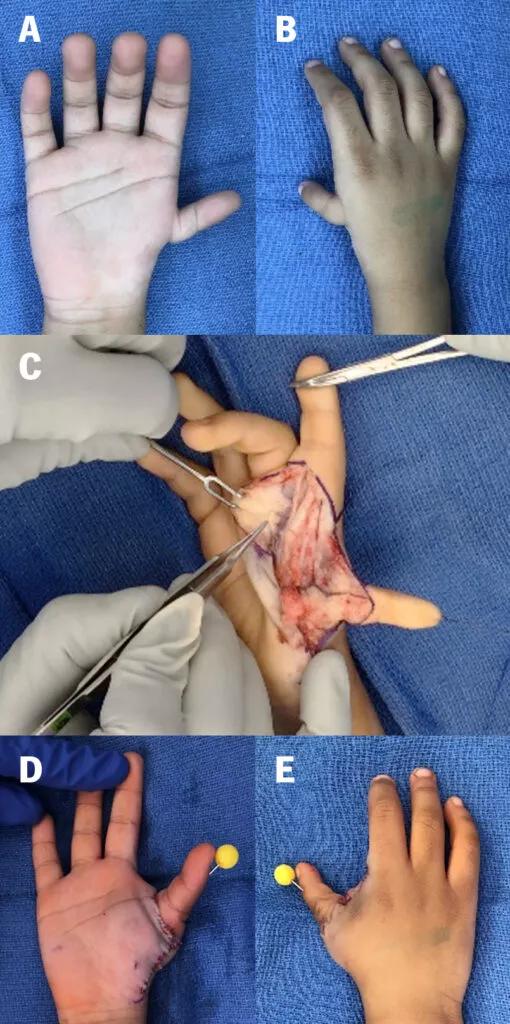
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d449e49b-98cc-4d7c-b4ce-596c53369dbc/22-ORI-3183860-CQD-Combo-Inset-4-510x1024_jpg)
Figure 3. Volar and dorsal views of a right hand with type IIIB hypoplastic thumb (A,B). Intraoperative view of the neurovascular structures dissected (C). Volar and dorsal views of the hand after pollicization (D,E).
Temporary stabilization is provided by suture and K-wire fixation. Again, long arm cast immobilization is recommended for six weeks followed by one month of foam splint protection. Functional use of the hand proceeds with occupational therapy as well as through use and experimentation as the child develops. The video below shows a patient using her hand to manipulate foam blocks with fine pinch six weeks after pollicization surgery.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/kWmTrOXWQik?feature=oembed)
Outcome of pollicization surgery.
Precise timing for initiation of surgical intervention in thumb hypoplasia has been debated. However, with our extensive congenital hand reconstruction experience, we have found that the earlier we can safely begin intervention, the more readily the child incorporates their new hand function into everyday activities.1-5,10,15 Some surgeons have recommended waiting until the child is as old as age 5 or 6, but this appears to be due to surgeons’ comfort with operating on larger structures.
We must remember that hands are the “antennae” of the developing child. Children use their hands to explore their universe and manipulate objects. As they demonstrate developmental milestones, the brain’s cerebral cortex develops an image of the hand and thumb and incorporates experiences into enhancing hand function.
We have found that commencing reconstruction of thumb function is most effective as early in development as possible. Ideally, this includes assessment shortly after birth, with the first stages of surgery as early as six months following full gestation. As surgical intervention may require more than one stage, our goal is to provide a child with a working, functional thumb before they begin preschool.
We follow patients throughout childhood to ensure maintenance of function while assessing their need for education, rehabilitation or surgical adjustments. Secondary surgery is required only occasionally.
Our patients have demonstrated exceptionally fine prehensile skills and effective function. They have participated in and mastered activities including sports, musical instrument performance, the arts and skilled technical endeavors throughout childhood and beyond.
Drs. Styron and Seitz are hand and upper extremity surgeons in the Department of Orthopaedic Surgery at Cleveland Clinic.
References
Advertisement
Radiation therapy helped shrink hand nodules and improve functionality
Noninvasive treatment may slow progression of Dupuytren's disease and plantar fibromatrosis
How it’s similar but different from the direct anterior approach
Collaboration must cross borders and disciplines
Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols
Should surgeons forgo posterior and lateral approaches?
How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians
Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes