Finally, a solution after multiple revision surgeries for delayed bone healing, loose hardware and unrelenting infection
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/Pd_hnGcekgo?list=PLMG0zKOgNqNmjblpUju0Zf0_AgXDo3Tib)
Vascularized Fibular Graft for Nonunion of Humeral Shaft Fracture (Graphic)
After a ground-level fall, a 64-year-old woman sustained a comminuted proximal humerus fracture with radial nerve injury. A non-Cleveland Clinic surgeon repaired the fracture with an intramedullary nail. However, healing was delayed, and eventually the patient was found to have deep infection. The patient underwent a cleanup procedure, but seven months later she required removal of the intramedullary nail due to nonunion and loose hardware.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The patient had a revision surgery including open reduction and internal fixation (ORIF) with an anterolateral plate and intravenous (IV) antibiotics. Although the radial nerve function recovered in the next six months, the patient returned with increased swelling and loosening of the screws.
She then had partial hardware removal and another round of IV antibiotics followed by a second revision ORIF through a posterior approach (Figure 1).
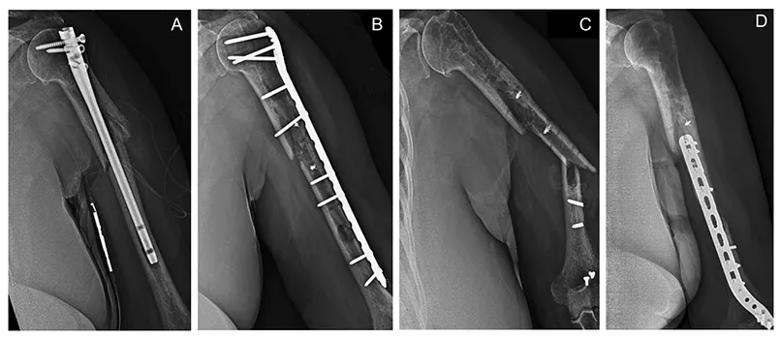
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1a6f1fe5-06f2-482d-8103-6318ba337e73/23-ORI-3860256-CQD-Inset-1_jpg)
Figure 1. Radiographic diary of surgeries prior to presentation at Cleveland Clinic. The patient had intramedullary nail for original fracture (A), followed by a washout and ORIF using an anterolateral plate (B) that went into nonunion (C), requiring removal of hardware, IV antibiotics and revision ORIF using a posterior approach (D).
The patient did well for 10 months but then felt a pop in her arm while buckling a seatbelt, followed by increased pain and clicking in her arm. X-rays showed loosening of the distal screws. That’s when the patient, now 66 years old, presented at Cleveland Clinic. Advanced imaging revealed nonunion of the fracture with no evidence of callus formation, and multiple areas of broken or loose hardware.
In the above video, shoulder and elbow surgeon Vahid Entezari, MD, of Cleveland Clinic’s Department of Orthopaedic Surgery, explains his strategy for treating this patient with persistent atrophic nonunion and loosening of hardware.
“This was a challenging case because of lack of bone healing and multiple incidents of failed hardware,” he says. “The patient had several surgeries and most likely persistent infection. Our treatment strategy was to stage her surgeries to first address the persistent infection and then tackle the atrophic nonunion with ORIF of the fracture and a vascularized fibular graft.”
In Stage 1, the orthopaedic team at Cleveland Clinic removed all the hardware, including retained anchors and broken screws; filled the bone defects with antibiotic-impregnated ceramen; and treated the patient with a cast and six weeks of IV antibiotics (Figure 2A).
Advertisement
In Stage 2, the team performed a shortening osteotomy and ORIF of the fracture using a titanium locking plate with multiaxial screws through a posterior approach. They packed the site with bone marrow aspirate and demineralized bone matrix. The patient then was repositioned, and a plastic surgery team harvested a vascularized fibular strut graft from the patient’s ipsilateral leg. The orthopaedic team fixed the strut graft to the humerus shaft using two cerclage tapes through an anteromedial approach (Figure 2B). The graft then was connected to the arm vasculature (Figure 2C).
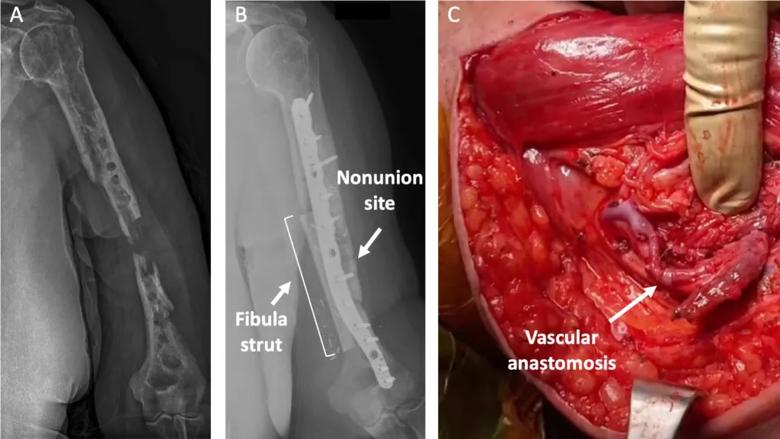
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/291910b3-cfa6-448a-b3c8-3064e9257b14/23-ORI-3860256-CQD-Inset-2-1024x576_jpg)
Figure 2. Radiographic studies of the staged surgeries. The patient had extensive debridement and removal of loose hardware followed by IV antibiotics (A). She then had shortening osteotomy and ORIF of the fracture using plate osteosynthesis through a posterior approach. In addition, a vascularized fibula autograft was added to augment the fixation through an anteromedial approach (B). Blood was supplied to the graft from the brachial artery through an anastomosis (C).
At one-year follow-up, the patient’s arm and leg incisions had healed with no complications. The patient reported no pain, great range of motion and 90% function in her upper extremity (Figure 3). She was able to use her arm to perform activities of daily living with minimal limitation and was extremely happy with her outcome.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/94f0b003-5be9-4a1c-8261-a45405009e4a/23-ORI-3860256-CQD-Inset-3_jpg)
Figure 3. The patient’s range of motion at one-year follow-up.
Advertisement
Advertisement
Falling from standing height should not break bones
Trauma patients present with infected pilon and distal femur fractures
How it’s similar but different from the direct anterior approach
Collaboration must cross borders and disciplines
Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols
Should surgeons forgo posterior and lateral approaches?
How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians
Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes