Immunotherapy is preferred initial treatment for majority of patients
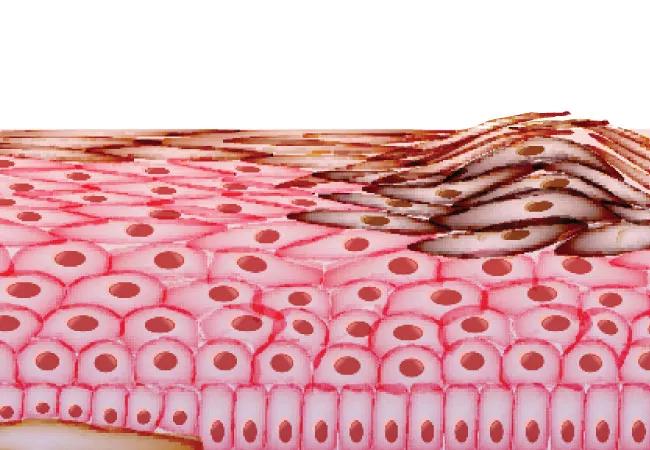
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/70e1a59a-193e-4a1f-ac8f-c4e0d0c49d1c/22-CNR-3405610-CQD-Hero-650x450-Dr-Funchain-melanoma_jpg)
melanoma
Combination nivolumab/ipilimumab increases overall survival when used prior to BRAF and MEK inhibitor therapy, according to a recent study presented at ASCO’s new Plenary Series. The researchers established that in stage 4 patients with the BRAFV600 mutation, using nivolumab/ipilimumab first resulted in a 20% absolute improvement in two-year overall survival (72% vs. 52%) compared to dabrafenib/trametinib. Progression-free survival and durability of response was also improved using this first-line immunotherapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Roughly 50% of patients with metastatic melanoma have the BRAFV600 mutation. Although checkpoint inhibitor immunotherapy and targeted therapy both demonstrate clinical benefits for these patients, clinicians have long struggled to determine the appropriate treatment sequence. The results of the DREAMseq trial made it clear that for the majority of patients, combination nivolumab/ipilimumab, followed by BRAF and MEK inhibitor therapy if needed, is the preferred treatment sequence.
“In the past, it was common to see decisions made in terms of either practitioner or patient preference,” says Pauline Funchain, MD, DREAMseq co-author and an oncologist/cancer genomics expert at Cleveland Clinic. “Since targeted therapy is oral, patients often preferred this option, but there are now real data showing that this population of patients can live longer if they start with immunotherapy and then use targeted therapy. This is a true practice-changing study.”
In this two-arm, phase 3 trial, patients had measurable, unresected stage 3 or 4 melanoma containing the BRAFV600E/K mutation. Eligible patients were treatment naive for metastatic disease, but may have received adjuvant therapy that did not include a programmed cell death protein, cytotoxic T-cell, lymphocyte-4, BRAF or MEK inhibitor. A total of 265 patients with BRAFV600-mutant metastatic melanoma were randomly assigned to receive either combination nivolumab/ipilmumab (arm A) or dabrafenib/trametinib (arm B). At disease progression, they then switched to the alternate therapy, dabrafenib/trametinib (arm C) or nivolumab/ipilimumab (arm D).
Advertisement
Each patient received nivolumab 1 mg/kg and ipilimumab 3 mg/kg once every three weeks for four doses followed by nivolumab 240 mg intravenously once every two weeks for up to 72 weeks (arms A and D) or dabrafenib 150 mg twice a day and trametinib 2 mg orally once daily until disease progression (arms B and C). In 2019, investigators were given the option to switch to alternate induction doses of nivolumab 3 mg/kg and ipilimumab 1 mg/kg once every three weeks for four doses for arms A and D.
The two-year overall survival for patients starting on arm A was 71.8% and arm B was 51.5%. The objective response rates were:
Median duration of response was not reached for arm A, and was 12.7 months for arm B.
Dr. Funchain noted that BRAF testing should be performed uniformly for all patients with melanoma prior to determining the course of treatment. “Incorporating this extra step can take time, but it really matters which treatment to start with,” she says.
There are many ways to test for mutations. Clinicians may choose to perform immunohistochemistry (IHC), which identifies roughly 95% of mutations and can be done in 24 hours in some cases, or DNA sequencing, which can additionally identify rare mutations and takes two to three weeks. If the IHC is negative, the next step is to perform sequencing to confirm that the other 5% of mutations are not missed.
The DREAMseq study focused on stage 4 patients, but due to enrollment logistics did not include those who were acutely ill. Dr. Funchain was quick to point out that there are still unknowns about this population. “For very fast-growing stage 4 BRAF-mutant melanoma, some key opinion leaders would say that population might be better to start with targeted therapy because it tends to work very quickly, though the jury is still out on what works best for those patients.”
Advertisement
Many questions also remain about whether targeted therapy or immunotherapy is the right initial treatment for patients at earlier stages of disease. “Immunotherapy can have permanent side effects such as hypothyroid or adrenal insufficiency, so there is a real concern about putting patients with fully resected disease who are considering adjuvant therapy at risk of permanent side effects when surgery could have been curative,” says Dr. Funchain. “It’s possible that targeted therapy may be the right first course of action but in that population, we don’t know yet which is better in terms of overall survival.”
In the future, the researchers hope to answer further questions, such as:
“We now know that in these melanoma cases, it matters which therapy you start with,” says Dr. Funchain. “As we learn more, this question will certainly come up with other cancers entering into the immunotherapy treatment arena.”
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Neoadjuvant immunotherapy improves outcomes
Largest study of its kind identifies three treatment exposures that contribute to risk
Family history may eclipse sun exposure in some cases
Timing of adjuvant immunotherapy unclear for maximum overall survival
Melanoma may be more heritable than we think
Highly personalized treatment shrinks tumors resistant to immunotherapy
Cleveland Clinic Cancer Institute among select group of centers to administer highly personalized treatment