Telehealth aids in treatment of fibromyalgia and median arcuate ligament syndrome

More than three years after COVID-19 jumpstarted telehealth, Cleveland Clinic’s Department of Pain Management continues to see the benefits for patient care. This is especially true in disease processes where patient education plays a critical role in proper management.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“In my own practice, we find telehealth visits especially useful for fibromyalgia and median arcuate ligament syndrome,” says Benjamin Abraham, MD, a pain medicine specialist. “These rare and often misunderstood conditions require a well-informed patient to avoid the many pitfalls, including unnecessary procedures or surgeries.
A lot changed with COVID-19, says Dr. Abraham. Although some pandemic-era policies on telehealth are likely to evolve, opportunities around virtual visits are expected to expand as clinicians explore new ways to standardize treatment, improve the patient experience and make healthcare more efficient.
Even before the pandemic shut down non-emergency care in 2020, Cleveland Clinic patients seeking help for fibromyalgia could take part in shared medical appointments (SMAs). Now virtual SMA visits support patients in several ways, says Dr. Abraham.
With limited variation in recommended treatments, patient education becomes one of the most important tools – which is why online interaction is so successful. Pain Management recommends any patient who comes in with a question about the diagnosis or treatment of fibromyalgia to attend a series of five SMAs with a small group (up to 10 patients).
“We’re going to cover all their questions and concerns,” says Dr. Abraham. “In some cases, through this process a person might find that they don’t even have this condition. If they do have it, they’re getting support in part because they hear what other patients have experienced.”
Advertisement
From a practical standpoint, telehealth can be especially helpful with fibromyalgia.
“Patients with this condition in particular are often increasingly home bound,” says Dr. Abraham.
“They may be having sleep dysfunction or mood problems. Oftentimes getting to an appointment is just not doable. They’re already having problems with other life responsibilities. The virtual platform is ideally suited to them.”
When fibromyalgia patients are seen individually in the office, he adds, it can take several visits to identify the breadth of symptoms they’re experiencing. They might not recognize that their diarrhea, migraines or sleep dysfunction are related to the condition. Instead, they spend time searching for specialists to treat those symptoms, and they become frustrated.
But when a patient hears an SMA presentation and other patients share their own experiences with those symptoms, the message is more likely to take hold.
“Patients don’t have to believe me,” says Dr. Abraham. “They can talk to nine other people in that visit. Social isolation is a big problem in this disease process, so the group experience can be powerful.”
Virtual SMAs have another advantage, he adds. While some patients who attended SMAs in person had concerns about privacy or were anxious in group settings, a virtual environment offers a layer of protection. Anyone can turn off their camera, and no one is required to speak.
“I can address each patient individually, having reviewed their chart already, and having made some notes myself,” says Dr. Abraham. “I might ask whether a patient has had certain symptoms, or whether these symptoms started at the same time as other, seemingly unrelated, problems. That can be a benign way to engage them in a more comfortable, semi-anonymous way.”
Advertisement
Video visits also have been especially helpful in caring for out-of-town patients referred for possible median arcuate ligament syndrome (MALS), a relatively rare condition in which the median arcuate ligament compresses the celiac artery and nerve. MALS can cause nausea and vomiting, weight loss, bloating, diarrhea, and postprandial pain. Some patients who have compression don’t have symptoms. Others have symptoms, but MALS is not the cause. For still others, MALS is comorbid with other conditions.
Not only can MALS be difficult to diagnose, but patients with these symptoms can have difficulty getting to the right provider.
“Because of the relative commonality of this incidental finding, these patients are being juggled among many subspecialists,” says Dr. Abraham. “So before traveling to one of the few centers of excellence for this condition in the country, the patient often wants to talk to someone for direction and guidance.”
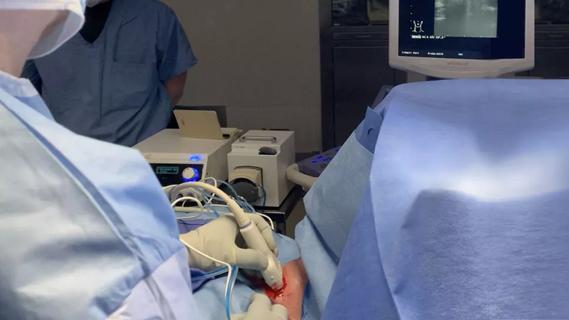
Video visits allow Cleveland Clinic specialists to do virtual screenings and coordinate any tests or imaging (typically CT scan and ultrasound) with the patient’s home doctor. In Cleveland, the patient may undergo a diagnostic celiac plexus block to confirm the MALS diagnosis and rule out other conditions of the gastrointestinal tract.
In addition to reducing travel stress through virtual visits, Cleveland Clinic has standardized the approach to all suspected MALS cases regardless of whether the patient initiates contact with specialists in pain management, vascular surgery, gastrointestinal surgery or a general surgeon.
Advertisement
“We’re all funneling these patients to one algorithm: confirmation of the condition by CT scan and ultrasound,” says Dr. Abraham.
“Surgical or interventional pain treatments might not be appropriate or effective for some patients,” he says. “That diverts medical resources and of course leads to frustrating office visits. Patients are best served in a setting where they get standardized care.”
Only after MALS is confirmed does the patient meet with a vascular surgeon to talk about treatment options.
Advertisement
Advertisement

Add AI to the list of tools expected to advance care for pain patients
Radiofrequency ablation significantly reduces symptom severity, shrinks nodules

Program enhances cooperation between traditional and non-pharmacologic care

A surgeon’s perspective: three patient groups

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Compassion, communication and critical thinking are key

Cleveland Clinic study investigated standard regimen