Baseline high-sensitivity cardiac troponins independently associated with cardiac events
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
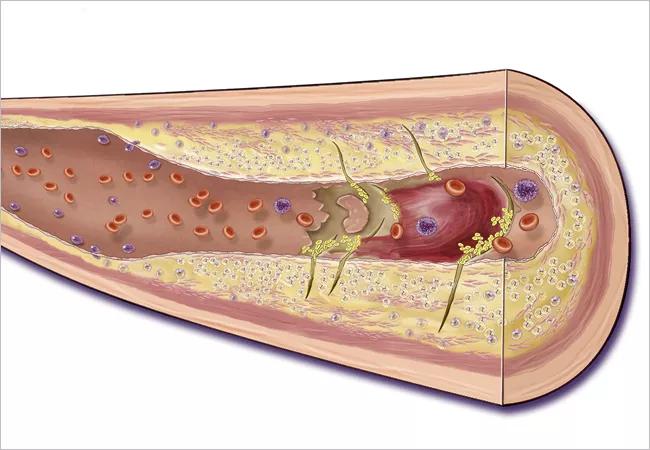
Patients with chronic systemic inflammatory states may be at increased risk of developing cardiovascular (CV) disease, which has implications for drug therapy and can put patients at risk of premature death. The ability to predict which patients with RA or OA are most likely to experience a major cardiac adverse event (MACE) may help rheumatologists risk stratify these patients early.
Although validated risk stratification methods exist, such as the Systematic Coronary Risk Evaluation (SCORE), Framingham risk score (FRS) and Reynolds risk score (RRS), they tend to underestimate CV risk in patients with arthritis. There remains a need to identify other prognostic indicators of CV risk to help mitigate this risk early on in this patient cohort.
High-sensitivity cardiac troponins (hscTnT) allow the measurement of cardiac troponin concentrations below conventional levels, and can be used to assess the severity of subclinical myocardial damage. Meanwhile, high-sensitivity C-reactive protein (hsCRP) is traditionally applied in CV risk stratification. In order to evaluate the prognostic relevance of these biomarkers, we evaluated data from the PRECISION biomarker sub-study, looking for associations between hscTNT, hsCRP and major adverse cardiac events. Our results were presented at ACR Convergence 2020.
We measured hscTnT and hsCRP in a subset of RA (N = 636) and OA (N = 6,269) patients in the PRECISION trial. The PRECISION trial was a randomized, controlled, non-inferiority clinical trial conducted worldwide involving patients who had RA or OA and increased CV risk. The primary CV outcome was major adverse cardiac events (MACE), which we defined as CV death, non-fatal myocardial infarction or non-fatal stroke, re-vascularization, hospitalization for unstable angina or transient ischemic attack) with at least 18 months of follow-up.
Advertisement
Within this cohort, 58% of patients were female, 80% were Caucasian, and the mean age was 63.6 ± 9.4 years. Eighty percent of patients in this cohort had hypertension, 36.5% had diabetes and 17.8% had known coronary artery disease.
Looking at the biomarkers, the median baseline hscTnT was 6.3 ng/L, and was similar in the RA cohort (5.6 ng/L) and the OA cohort (6.4 ng/L). Baseline hscTNT was a significant predictor of MACE during the 18-month follow-up for both patients in the RA cohort (HR 1.60; 95% CI 1.06, 2.41) and the OA cohort (HR 1.23; 95% CI 1.04, 1.46). The association between hsCRP levels and MACE was weaker for patients with RA (HR 1.36; 95% CI 1.05, 1.75) and not significant for patients with OA (HR 1.09; 95% CI 0.99, 1.21).
In this study, we found hscTnT to be independently associated with MACE in both RA and OA. Further prospective studies to address the predictive role of hscTNT for CVD events in RA and OA patients can expand preventive treatment strategies.
Given the increased CV risk in patients with chronic arthritic conditions, physicians should strive to actively manage traditional risk factors while optimizing disease control. Interventions aimed at modifying risk factors of coronary artery disease include smoking cessation, controlling cholesterol and weight, maintaining a healthy (perhaps anti-inflammatory) diet and moderate exercise.
Note: Co-authors include Daniel H. Solomon, MD, MPH; Mingyuan Shao, PhD; Katherine E Wolski, MPH; Steven E Nissen, MD; Stanley L Hazen, MD, PhD, and WH Wilson Tang, MD, on behalf of the PRECISION trial investigators.
Advertisement
Advertisement

First full characterization of kidney microbiome unlocks potential to prevent kidney stones

Researchers identify potential path to retaining chemo sensitivity

Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests

Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology