Tight disease control throughout pregnancy may improve outcomes

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
KC is a 36-year-old female with a past medical history of hypothyroidism and rheumatoid arthritis (RA). She was diagnosed with RA at age 33 when she presented with two months of swelling of her ankles and feet and was subsequently found to have a positive rheumatoid factor and anti-cyclic citrullinated peptide (CCP) antibodies, with florid inflammation on blood work. X-rays of her ankles and feet did not show evidence of erosions. She was placed on a course of prednisone and oral methotrexate; however, she was unable to tolerate methotrexate. She was switched to adalimumab 40 mg subcutaneously every two weeks, which was eventually increased to weekly dosing. She went on to achieve tight disease control on adalimumab therapy. At this time she was cleared to attempt conception. Shortly after finding out she was pregnant (estimated at 4 weeks gestation), she stopped adalimumab. She developed progressive stiffness and swelling of her joints. At an acute visit in our clinic, she had polyarticular swelling of hands and wrists, with synovitis throughout bilateral metacarpophalangeal joints.
Women with RA who are of childbearing age face many challenges throughout pregnancy and extending into the postpartum period, from fertility to birth outcomes and control of disease. With appropriate preconception counseling and tight control of disease activity, it is still possible to achieve good pregnancy outcomes for our patients. This is the topic of a recent review article published in Best Practice & Research: Clinical Obstetrics and Gynecology to raise awareness of this subject matter and update both rheumatologists and obstetricians. With new information available regarding outcomes and safety, physicians should feel renewed confidence to guide management in these patients.
Advertisement
Infertility rates are 2.3 times higher in women diagnosed with RA during childbearing years compared with those diagnosed after the completion of the childbearing years; however, there appear to be additional factors — besides infertility — contributing to the smaller number of pregnancies and births among women with RA. Research indicates that women with RA have fewer children than the general population for a number of physiological reasons including ovulatory dysfunction, endometriosis, alterations of cytokines (critical to embryonic implantation), aberrant functioning of T-cells, chronic use of NSAIDs or glucocorticoids. Some psychological factors include decreased sexual desire as well as concerns about their ability to care for children, that their medications might harm a developing fetus or that they might pass RA onto their offspring.
Research indicates that disease activity improves for about 60% of women with RA during pregnancy, and flares in 46.7% during the postpartum period. RA flares occurred in 29% of women, most commonly during the first trimester. Risk factors associated with these flares were active disease and elevated CRP in early pregnancy and the discontinuation of tumor necrosis factor inhibitors (TNFi). In this study, 20% of patients discontinued TNFi treatment when they received a positive pregnancy test. Disease flares can be treated during pregnancy; however, continuing TNFi treatment throughout pregnancy may help reduce the risk.
Many women are not provided with adequate information about the risks and benefits of continued therapy throughout pregnancy, nor are they educated on the medications that are safe for pregnancy. The use of anti-TNF therapy and other medications deemed safe for pregnancy is a newer concept; the American College of Rheumatology Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases was only recently released in early 2020. With this new information on hand, a thorough discussion about risks and benefits of continuing therapy needs to take place in the pre-conception period.
Advertisement
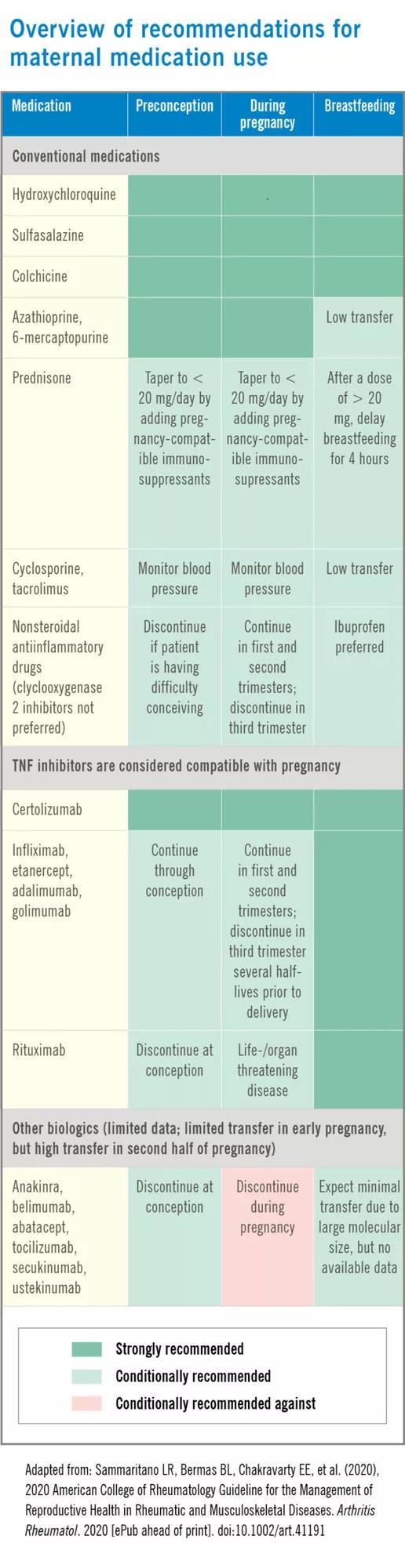
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/519a7832-4671-40b8-b860-57e31b0e6b4d/20-RHE-1870684-PregnancyRheumatoidArthritis_Littlejohn-800x3100-1-scaled_jpg)
Compared to the general population, pregnant women with RA have been shown to have a higher prevalence of hypertensive disorders, premature rupture of membranes, antepartum hemorrhage, preterm delivery, intrauterine growth restriction and cesarean delivery. Several studies suggest that tight disease control may improve birth outcomes.
Although further research is needed in this area, the literature should motivate rheumatologists and obstetricians to strive for low levels of disease activity before and throughout pregnancy.
Advertisement
Advertisement

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity

Psychological care can be a crucial component of medical treatment