Wait-and-see approach delays surgery until six weeks postpartum
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 23-year-old female presented for laryngology consultation in her third trimester of pregnancy. Her initial symptoms included burning throat pain and episodes of hemoptysis when sneezing or coughing. Prior to this consult, the patient had gone to the emergency room for an episode of hemoptysis at 20 weeks of gestation, and was evaluated by gastroenterology.
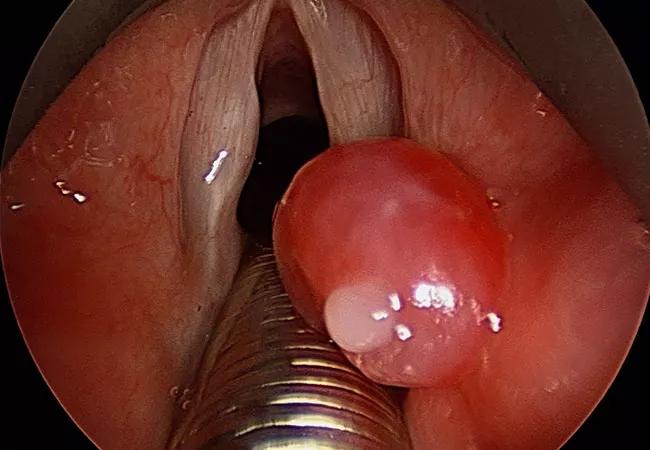
At 26 weeks of gestation, she had another episode of hematemesis, along with feeling short of breath and a globus sensation in her throat. She was referred to otolaryngology, and we evaluated her at 36 weeks of gestation. We examined her via flexibly laryngoscopy, and found a vascular, right false vocal fold neoplasm.
Concerned about the possibility of hemorrhage and/or further airway restriction before or during delivery, we created a treatment plan. With the advice of the high-risk obstetrics team, we decided that the patient should undergo elective induction at 38 weeks gestation in the high-risk obstetrical unit, with the otolaryngology service on standby with a difficult airway cart. Under the original plan, the patient was to have the laryngeal lesion excised the day following delivery.
Induction proceeded with no complications, and the patient decided against the scheduled laryngeal mass excision. The mass was removed six weeks later via suspension microlaryngoscopy using potassium titanyl phosphate (KTP) laser. The lesion was pedunculated and anchored on the medial right arytenoid mucosa with a hyper-vascular stock.
Advertisement
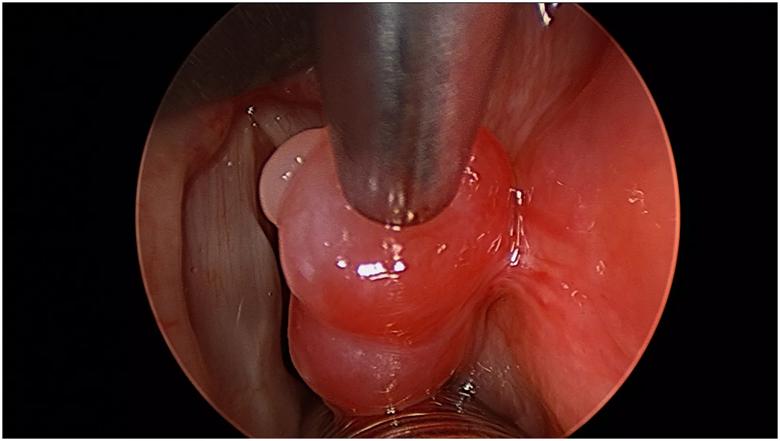
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b694bda9-9e95-4721-8cc4-18a002a4204e/image-2_jpg)
Intraoperative view, hyper-vascular stalk anchoring pedunculated lesion.
Pyogenic granuloma is a common, benign, vascular lesion in pregnancy, and tends to develop on the lip, nose, oral mucosa and tongue. It can occur at any age, but is more common in the second decade of a young female’s life. The oral pyogenic granuloma is smooth or globulated, and may appear as a small, red, pink or purple erythematous papule. Bleeding is a common symptom, and concern for hemorrhage was also an issue in this case.
Pregnancy-related pyogenic granulomas sometimes go away on their own following delivery, and often a wait-and-see approach is appropriate. This case was rare because of the location of the pyogenic granuloma. These lesions rarely develop on the larynx or trachea. When a pyogenic granuloma does develop in the airway, they are thought to be associated with past trauma to the area. Our patient did not have prior trauma to the larynx.
We were prepared to operate on our patient if her airway was further compromised, working closely with our high-risk obstetrics team. However, the patient’s episodes of hemoptysis were controlled conservatively, and, with regular monitoring, we were able to postpone surgical removal of the pyogenic granuloma until after delivery. The patient had no morbidity and follow-up exams show no evidence of recurrence.
Further research is needed regarding emergent airway management during pregnancy.
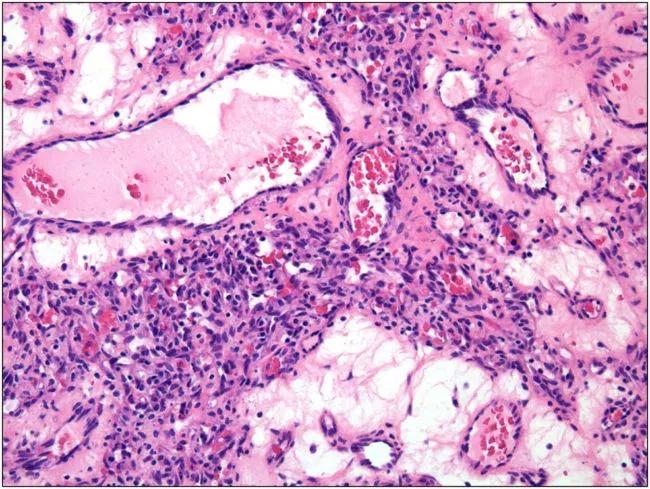
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6b9268e2-ddc3-4d16-a50f-ed6186747a5c/image-5-e1554124558719_jpg)
Lobular vascular proliferation of capillaries, 200x magnification.
Advertisement
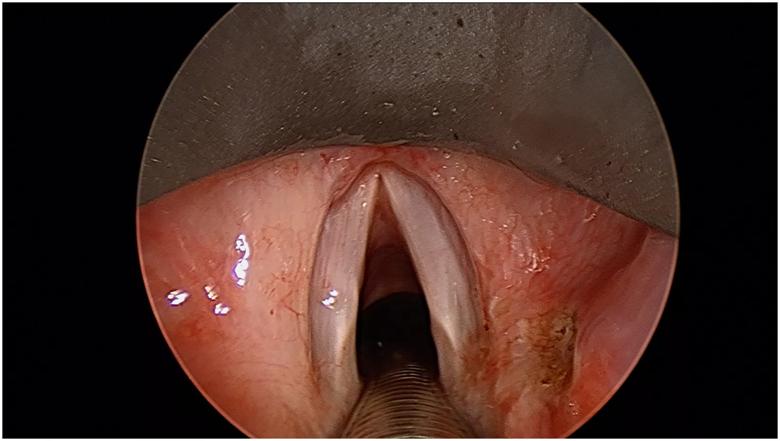
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2cecc300-5ad0-4ae9-91d0-bc449b5ebc0e/image-4_jpg)
Intraoperative view, post-excision
Note: Images used with permission from Elsevier; originally published in: Hanick AL, Meleca JB, Billings SD, Bryson PC. Pyogenic granuloma of the larynx: a rare cause of hemoptysis. Am J Otolarngol. 2019;40(2):331-333.
Advertisement
Advertisement

Multidisciplinary teams work together in in-situ scenarios

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity