Cleveland Clinic’s Rheumatic Lung Disease program treats patients with complex conditions

by Aditi Patel, MD, Sameep Sehgal, MD, Kristin Highland, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A female in her 60s was referred to our rheumatology clinic after she reported a history of new onset Raynaud phenomenon for two months. In addition, she reported hand puffiness, heartburn, dyspnea on exertion and a rash laterally over her thighs.
The examination revealed puffy hands, erythema around the nailbeds, rash over the lateral aspect of her thighs (above), weak proximal hip muscles, and crackles at the base of the lung fields. Laboratory evaluation was notable for elevated creatinine kinase at 2034 U/L, positive ANA, titer >1:1280, nuclear fine speckled pattern, and ribonucleoprotein antibody.
Additional workup included a magnetic resonance imaging (MRI) of her thighs, which showed myositis and computed tomography (CT) of the chest, which showed mild reticulation with ground glass opacity within the lower lobe peripheral lung fields. This was suggestive of interstitial lung disease (ILD) and reduction in diffusion capacity.
A skin biopsy was notable for interface dermatitis with increased dermal mucin and chronic perivascular inflammation. The patient also was noted to have absent esophageal contractility on manometry testing. With her constellation of symptoms, she was diagnosed with mixed connective tissue disease (MCTD) with features of overlap myositis.
MCTD describes a disorder characterized by features of systemic sclerosis, systemic lupus erythematosus and inflammatory myopathy. Typical symptoms include Raynaud syndrome, inflammatory arthritis, swollen hands, muscle weakness, difficulty swallowing, heartburn and dyspnea. Skin changes such as systemic sclerosis or lupus-like rashes also can be seen. Pulmonary involvement in the form of interstitial lung disease and pulmonary hypertension are often causes of mortality in these patients.
Advertisement
The patient was treated with high doses of corticosteroids, mycophenolate mofetil (MMF) and intravenous immune globulin. MMF was switched to intravenous rituximab every six months due to leukopenia. She had complete resolution of her respiratory symptoms, CT chest findings and myopathy.
Our patient was seen in Cleveland Clinic’s Rheumatic Lung Disease program, which involves a rheumatologist, pulmonologist and other subspecialists. Patients with pulmonary manifestations from rheumatic diseases such as systemic sclerosis and inflammatory myopathies receive comprehensive
care. This integrated team approach provides expertise for patients with multisystem complex diseases. Specialists with distinct areas of expertise deliver care efficiently and with the goal to improve patient outcomes.
The clinic also provides unique opportunities for clinical research and for trainees to be involved in understanding complex medical decision-making.
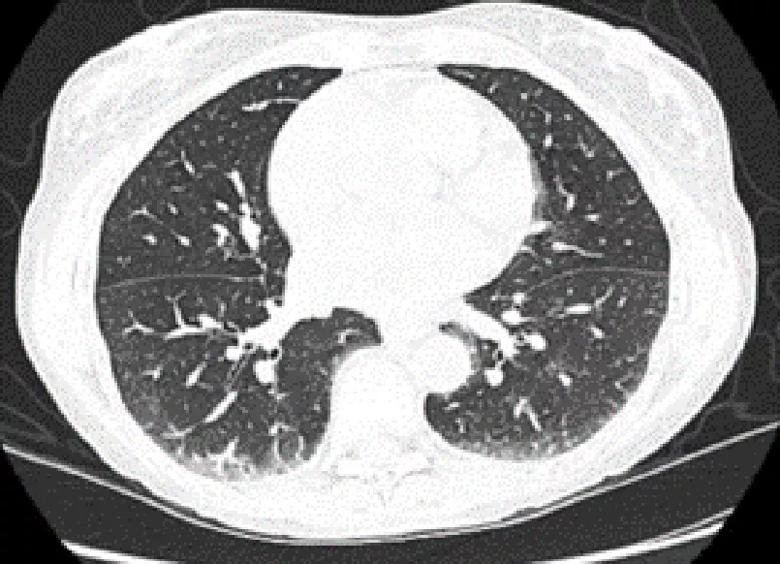
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1dfe371b-e589-4ed6-9d1d-7c49f03fdfc0/23-RHE-4333861-CQD-inset1-left_jpg)
Above, a CT chest scan shows changes of nonspecific interstitial pneumonia.
Below, complete resolution of CT findings can be seen at the patient’s one-year follow-up.
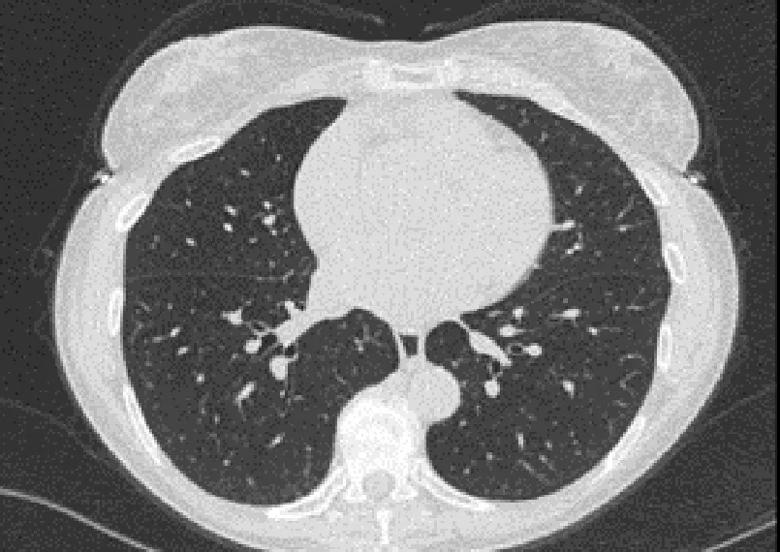
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7512d7d7-9c4f-4637-bca5-05081333aa7d/23-RHE-4333861-CQD-inset-2-right_jpg)
Advertisement
Advertisement

When to recommend aortic root surgery in Marfan and other syndromes
Many young patients can avoid lifelong anticoagulation with a valve-sparing approach

A review of treatment options for patients who may not qualify for surgery

Collaborative patient care, advanced imaging techniques support safer immunotherapy management

Rising rates in young miners illustrate the need for consistent prevention messaging from employers and clinicians

Multidisciplinary focus on an often underdiagnosed and ineffectively treated pulmonary disease

Management and diagnostic insights from an infectious disease specialist and a pulmonary specialist

Unraveling the TNFA receptor 2/dendritic cell axis