Case study illustrates the merits of virtual options for pre- and postsurgical care

These days, Cleveland Clinic neurosurgeon Peter Rasmussen, MD, conducts all his outpatient visits via telemedicine. While COVID-19 is what led him to go fully virtual for outpatient care, Dr. Rasmussen is no newcomer to virtual visits: He’s been conducting them for more than six years, and about 20% of his practice in Cleveland Clinic’s Cerebrovascular Center was virtual even before the pandemic. Now that mix is 90% virtual and 10% in-person, with the latter proportion devoted to actually performing surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“In a cerebrovascular practice, whether for a neurosurgeon or a neurointerventionalist, about 90% of practice today can be done virtually,” says Dr. Rasmussen. To illustrate, he shared the case of a recent patient he’s managed from afar — except for a two-day visit to Cleveland Clinic for surgery this past summer.
The patient is a 71-year-old woman from the U.S. West Coast who, in early 2019, was found to have asymptomatic left carotid artery stenosis with an isolated hemisphere. She had a history of hypertension and coronary artery disease for which she had received several coronary stents in prior years.
In 2019 she underwent carotid artery stenting at a local academic medical center, after which follow-up ultrasound and CT angiography revealed recurrent stenosis. Myointimal hyperplasia was suspected due to the angiographic appearance and early nature of the restenosis.
Repeat stenting was recommended by her local provider, but when she requested that it be done under anesthesia due to significant pain she had experienced during the first procedure, the provider refused. She sought alternate providers, and her search led her to Cleveland Clinic.
Based on initial phone conversations with Cerebrovascular Center staff, she was cleared for evaluation at a virtual visit with Dr. Rasmussen in late March 2020. Using a secure web link, she uploaded imaging studies from her local institution for review by Dr. Rasmussen during the virtual visit. The latter was conducted as a MyChart® video visit using Zoom™ for Telehealth, a HIPAA-compliant service integrated with Cleveland Clinic’s electronic health record (EHR) and MyChart online platform for patients.
Advertisement
The uploaded images — her most recent CT angiogram and angiograms from her initial carotid stent procedure — allowed Dr. Rasmussen to confirm severe recurrent stenosis in the isolated hemisphere. He told the patient he could perform repeat carotid stent placement in patients like her, and he assured her that anesthesia was not contraindicated and could be offered.
Although the severity of the patient’s stenosis qualified her procedure as nonelective, she was wary of traveling to Cleveland in the early weeks of the pandemic. During that period, she kept in touch with Dr. Rasmussen and his nurse via phone calls and messages through Cleveland Clinic’s MyChart platform, posing questions about the type of anesthesia to be used and the pre-admission process.
These interactions helped convince her to proceed with the stent placement at Cleveland Clinic, which was scheduled for July 2020. The patient flew to Cleveland and had another virtual visit with Dr. Rasmussen via video while she was in the anesthesia preoperative assessment clinic the day before her procedure. Placement of the carotid stent by Dr. Rasmussen was straightforward and successful (see Figures 1 and 2), and the patient was discharged the next day.
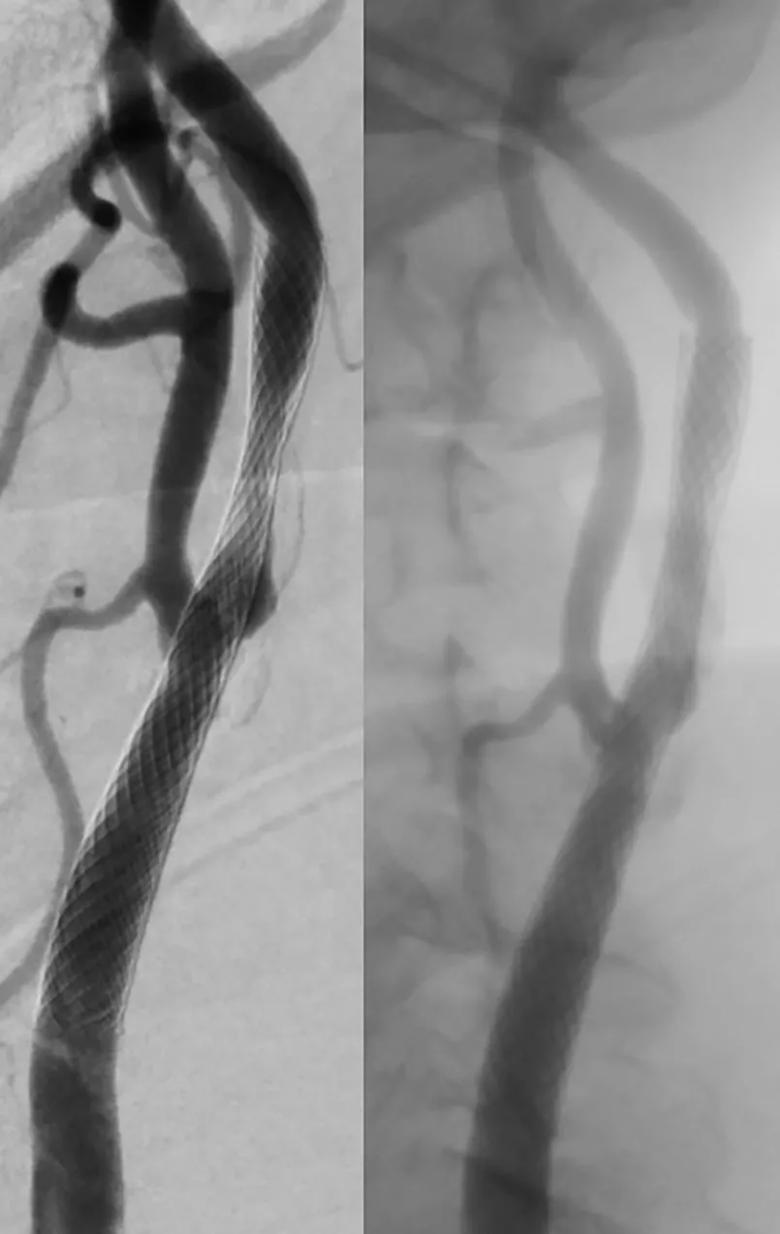
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4c8d09f7-49e4-4ba4-9513-edd65d7b9a7c/20-NEU-1917444_stenting-for-carotid-restenosis_jpg)
Figure 1. CT angiograms taken immediately before (left) and after (right) the patient’s carotid stent procedure at Cleveland Clinic. Note the significant narrowing of the artery at the area of hyperplasia in the preprocedure image and its correction following new stent placement.
Advertisement
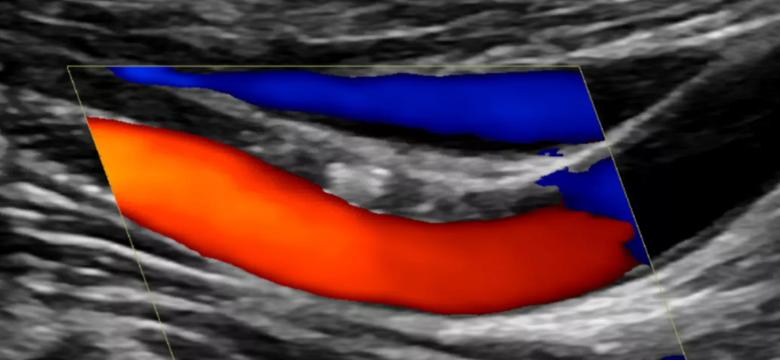
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8e15c15f-e233-4044-b341-b2e22a0a9e1b/20-NEU-1917444_carotid-ultrasound-after-angioplasty_805x372_png)
Figure 2. Carotid ultrasound taken the day after stent placement at Cleveland Clinic. The Doppler signal shows wide artery dilation with good laminar flow through the area of angioplasty.
The patient has fared well in the subsequent months, with no clinical complaints. She was instructed to follow up with her local provider, who was kept informed at each stage of her Cleveland Clinic management via letters generated through the EHR. She will undergo a follow-up ultrasound from a local provider six months after the procedure, with results sent to Dr. Rasmussen.
If the patient were to need additional imaging or a relevant blood test back in her West Coast community, Dr. Rasmussen would be able to simply route the order through the Epic EHR to a participating national imaging network or lab testing network, if the patient and her insurer were amenable to that.
Dr. Rasmussen, who served as Cleveland Clinic’s Medical Director of Distance Health for six years in addition to his neurosurgery practice, says he has observed three major changes over his six years of conducting virtual visits:
Advertisement
At this point, he says, the biggest potential barrier to wider adoption of virtual visits and telemedicine in general is regulatory in nature, as U.S. providers wait to see whether government ultimately revisits some of the easing of regulatory and payment rules enacted early in the COVID-19 pandemic.
“The technology is no longer a barrier in a neurosurgery practice like mine, so long as there is portability of imaging,” Dr. Rasmussen concludes. “This case and countless others illustrate that patients with many types of disease processes — cerebrovascular or other — can be very well managed over time at great distances using digital technologies. This gives patients more options and greater convenience, requiring them to travel to a facility only when truly necessary, such as when hands need to be laid on for evaluation, an image needs to be generated, blood needs to be drawn or a scalpel needs to pierce the skin.”
Advertisement
Advertisement

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does