Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH
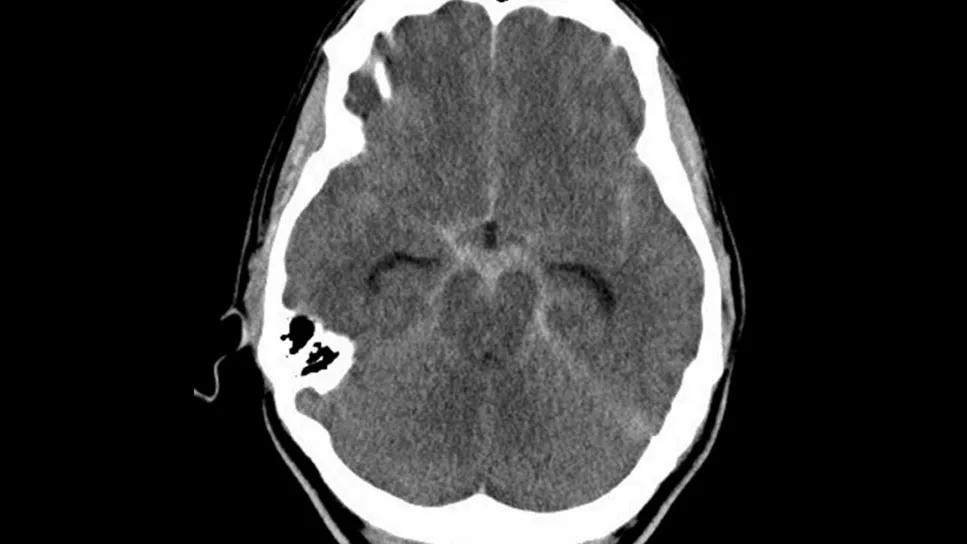
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9142c803-53de-4b60-a324-54cc7c7527cd/scan-showing-perimesencephalic-subarachnoid-hemorrhage)
brain scan showing perimesencephalic subarachnoid hemorrhage
Evaluation with digital subtraction angiography (DSA) to assess “benign” perimesencephalic subarachnoid hemorrhage (PMSAH) is still warranted in addition to computed tomography angiography (CTA) in the search for an underlying ruptured aneurysm. After complete assessment, a patient with nonaneurysmal PMSAH without hydrocephalus can be managed with a shorter hospital stay and less strict monitoring, as clinical outcomes tend to be favorable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So concluded Cleveland Clinic investigators after analysis of a 15-year institutional series of 81 patients with PMSAH, the largest published series of its kind that included patients within the last decade. It recently appeared in Stroke: Vascular and Interventional Neurology (Epub 2024 Feb 19)
“In our series, 6.2% of patients had an underlying ruptured aneurysm, more than half of which were detected only by DSA,” says Cleveland Clinic interventional neurologist Gabor Toth, MD, the study’s senior and corresponding author. “Although the number was small, consequences of an occult ruptured aneurysm can be grave, justifying the continued need for this conventional and more invasive test.”
PMSAH is commonly referred to as benign because a source of bleeding often cannot be identified and recovery is usually uncomplicated. But in rare cases, an initially undetected ruptured aneurysm is the culprit. Investigation usually begins with CTA, often followed by DSA — a more invasive test considered to be the gold standard for detecting an intracranial vascular lesion. As CTA technology has advanced, the need for DSA investigation has been called into question.
Another controversy surrounding PMSAH is how intensively patients must be observed when no underlying ruptured aneurysm is found. The importance of other findings, such as vasospasm and hydrocephalus, is poorly understood. When vasospasm or hydrocephalus is symptomatic, patients may be hospitalized for extended times for monitoring and treatment.
Advertisement
This retrospective study was designed to help shed light on these issues by analyzing presentation, imaging findings and outcomes in a large series of patients with PMSAH.
The series consisted of 81 patients with PMSAH treated at Cleveland Clinic from 2007 to 2022. Mean age was 55.5 ± 10.3 years.
All patients had a baseline noncontrast head CT, CTA and DSA. CT was repeated for clinical deterioration. DSA was repeated for clinical deterioration or if vasospasm had been diagnosed. If no underlying ruptured aneurysm was detected by initial angiogram, repeat DSA was done after 7 to 10 days.
An underlying ruptured aneurysm was diagnosed in a total of five patients (6.2%). Of these, the aneurysm was detected only by DSA in three patients (3.7%) (two on the initial DSA and one on follow-up).
All aneurysms identified were in the posterior circulation (four were in the vertebrobasilar system and one was on the posterior communicating artery); four were saccular and one was a dissecting pseudoaneurysm. All aneurysms were small (< 5 mm in size).
Complications among the 81 patients included the following:
Advertisement
The primary end point was favorable functional status at discharge, defined as a score of 0 to 2 on the modified Rankin scale, indicating no to slight disability. It was achieved by 40% of those with an underlying ruptured aneurysm versus 91% of those with nonaneurysmal PMSAH (P = .01).
Unfavorable clinical outcomes were associated with the following:
All patients who had asymptomatic vasospasm alone without underlying ruptured aneurysm achieved favorable outcomes.
Dr. Toth emphasizes that this study provides support for two major practices in the assessment and care of patients with apparently benign PMSAH:
Dr. Toth adds that several baseline patient factors were significantly associated with having an underlying ruptured aneurysm: being a smoker, having a higher score on the Hunt and Hess scale, and having a higher modified Fisher grade. “For patients with such a profile, it is especially important to thoroughly investigate with DSA,” he notes.
Advertisement
He adds that there is currently insufficient evidence to forgo DSA in this patient population. “Unless the aneurysm detection rate with CTA reaches 100%, missing even one or two real aneurysms is a major concern with potentially life-threatening consequences,” Dr. Toth concludes.
Advertisement
Advertisement
Results may refine surgical selection criteria and advance clinical trial design
ENRICH trial marks a likely new era in ICH management
A case study in pairing imaging acumen with subspecialty expertise to yield answers and symptom relief
Technology helps address gait abnormality in normal pressure hydrocephalus and more
Large analysis of familial cases and genomic studies sheds light on genetic contributions
Cleveland Clinic-pioneered repair technique restores a 61-year-old to energetic activity
Retrospective study examines outcomes associated with common treatment pathways
Quick and aggressive responses to multiple complications have led to remarkable recovery