Helping patients avoid hyperglycemia

By Keren Zhou, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hyperglycemia is a risk factor for prolonged hospitalization and mortality. Because the period immediately after IV insulin infusion (IVII) discontinuation is one in which patients are prone to rebound hyperglycemia, some of our staff from the Department of Endocrinology, Diabetes and Metabolism joined colleagues from Cleveland Clinic’s Medical ICU (MICU) to take a closer look at this period.
There has been a dearth of knowledge concerning how to best transition patients in the MICU from IVII to subcutaneous (SC) insulin. To date, the vast majority of information on transitioning has been derived from the surgical and cardiothoracic ICUs. As a consequence, this period of time represents an opportunity for further study and possible intervention. Our team chose to conduct this study because of this paucity of information.
The study looked retrospectively at the transition from IVII to subcutaneous (SC) insulin in the Cleveland Clinic MICU. Patients included had received IVII in our MICU between June 2013 and January 2014. These patients were further divided into three cohorts based on the method (or lack thereof) of transitioning: no basal insulin used in the 24 hours before or after IVII discontinuation (NB), incorrectly given basal insulin (IB), and correctly given basal insulin (CB) [see Figure 1 below].
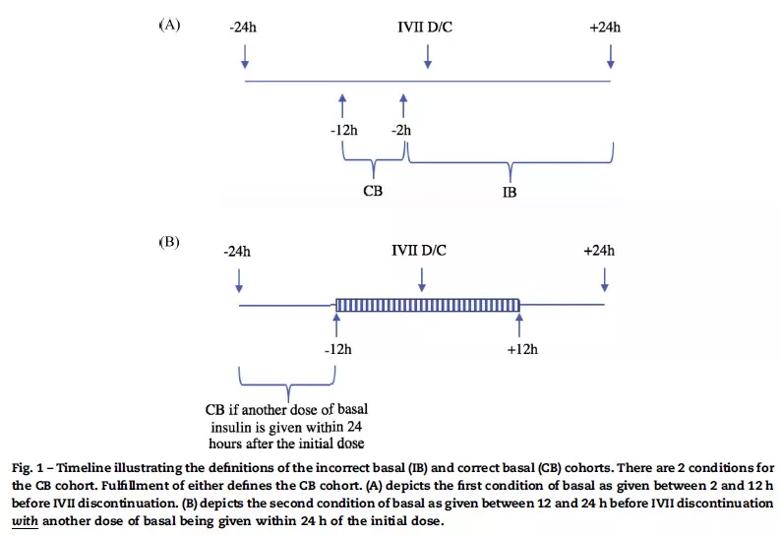
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/958e5916-6582-43f6-be88-f1f633d709ee/InsulinFigure_jpg)
There were 269 patients in total (NB 166; IB 45; CB 58). The study revealed that the NB cohort had the best blood glucose (BG). These individuals also had lower HbA1c, less pre-existing diabetes, and were less likely to be on home insulin as compared with individuals in the cohorts who had received basal insulin. This finding is consistent with prior data demonstrating that not all individuals who require IVII will go on to require SC insulin. The CB and IB cohorts both had similarly uncontrolled BG in the 24 hours post-IVII discontinuation, although the CB cohort trended towards better BG. This was likely being driven by the fact that the amount of insulin being provided was significantly less than what has been previously studied and recommended for transitioning from IVII (a traditional percentage-based method of calculating the dose of basal insulin by using 80 percent of the extrapolated 24-hour total of IVII).
Advertisement
It was also notable that significant numbers in the CB and IB cohorts experienced hypoglycemia in the first day after the IVII was discontinued. In review, many of these events were triggered by excessive bolus being given in an effort to correct hyperglycemia.
This retrospective study revealed real world deficiencies in the way that patients are being transitioned in the MICU, from receiving suboptimal doses of insulin to inappropriate timing of basal insulin. This is further compounded by the effort required post-IVII to correct the errors that occurred at the time of transition and, consequently, an increased number of hypoglycemic events.
The study led to questions of how we can improve our current practices, and the study team is currently in the process of designing a prospective study to follow up on this data by investigating a new method of transitioning in the MICU.
Dr. Zhou is a fellow in the Department of Endocrinology, Diabetes and Metabolism.
Advertisement
Advertisement

Pheochromocytoma case underscores the value in considering atypical presentations

Advocacy group underscores need for multidisciplinary expertise

A reconcilable divorce

A review of the latest evidence about purported side effects

High-volume surgery center can make a difference

Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D

Patients spent less time in the hospital and no tumors were missed

A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications