Understudied Src Family Kinase may serve as a potential therapeutic target
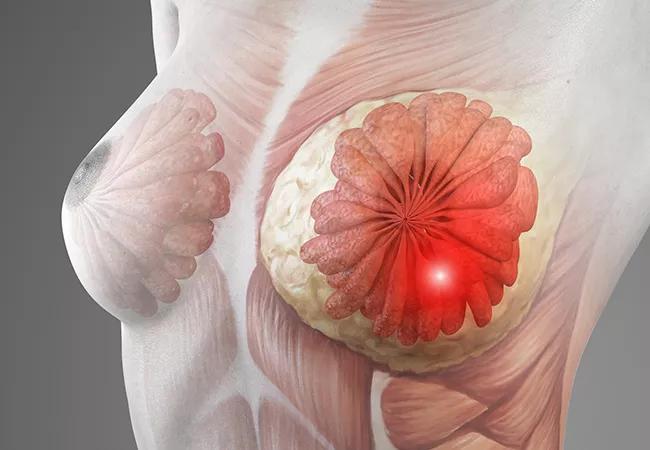
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e878a844-4525-4389-a6d3-3f5cd67697ef/21-CNR-2494210-CQD-650x450-1_jpg)
Breast Cancer
Investigators from Cleveland Clinic’s Lerner Research Institute and Case Western Reserve University have found that the sustained expression of YES1, a member of the Src family of protein tyrosine kinases (SFKs), plays an important role in the growth, viability and genomic stability of triple-negative breast cancer (TBNC) cells. The study further found that transient silencing of the YES1 gene leads to a significant reduction of TNBC cell growth and an increase in apoptosis. Early results of this research were presented at the 2021 San Antonio Breast Cancer Symposium (SABCS) held December 7-10 in Texas.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In explaining the motivation behind this research, Cleveland Clinic researcher and study coauthor Ruth A. Keri, PhD, notes that TNBC is a highly aggressive disease with limited therapeutic options. The disorder, which disproportionately affects Black women and young women, represents about 15% of all breast cancers.
“TNBC is very difficult to manage,” explains Dr. Keri. “There are several targeted treatments that can be added to the chemotherapy regimen, including immunotherapy and PARP inhibitors, but these drugs only work in a small percentage of patients.” Unlike hormone receptor-positive and HER2-positive breast cancers, TNBCs do not have estrogen, progesterone or HER2 receptors and, therefore, do not respond to many typical breast cancer therapies. Thus, there is an unmet need to identify better treatments for this aggressive disease.
In their search for potential new therapeutic targets for TNBC, Dr. Keri’s team focused on SFKs. The SFK family consists of nine non-receptor tyrosine kinases that play important roles in regulating cell growth, survival, mitosis and motility.
“These proteins are particularly important in cancer…and five of them are active in breast cancer,” explains Dr. Keri. “The assumption has been that these kinases all work the same way and do the same thing; however, it’s recently become clear that they actually operate quite differently, and some of them are even antagonistic.”
An interrogation of the data set published in the scope of the Cancer Genome Atlas project revealed that, of the five SFKs active in TNBC, YES1 was most frequently overexpressed. Using in vitro cell line experiments, Dr. Keri and her collaborators suppressed YES1 expression to better examine the function of this kinase in TNBC.
Advertisement
“We found that TNBC cells are actually very dependent on YES1 expression. In fact, if you remove the gene, the cancer cells stop growing,” she says, “That’s a good sign because it tells you that a drug capable of inhibiting YES1 may be very effective in this disease.”
In addition to a reduction in cell growth and an increase in apoptosis, loss of YES1 expression caused signs of chromosomal instability in TNBC cells, including double-strand DNA breaks, micronucleation, multinucleation and the appearance of dysmorphic nuclei. RNA-based experiments further found that the loss of YES1 function leads to alterations in DNA repair, replication stress and mitotic pathways.
“What we found is that YES1 was really important for maintaining the genomic blueprint for TNBC cells,” Dr. Keri explains.
Interestingly, the team’s earlier experiments of YES1 inhibitors in mice found that inhibition of the kinase did not negatively influence the health of the animals. This finding was expected because YES1 is not as highly expressed in healthy cells.
Dr. Keri emphasizes that the goal of TNBC treatment is to kill all cancer cells at once. “A lot of patients respond well to chemotherapies, and about half will be essentially cured — but the disease can quickly return in others.”
Dr. Keri’s team is now exploring whether treating TNBC with a combination of a YES1 inhibitor and chemotherapy might do a better job of eliminating the cancer cells upfront. Along these lines, their latest experiments are focused on testing a combination treatment consisting of a YES1 inhibitor and paclitaxel in mouse models of TNBC. Their preliminary studies suggest that that these two drugs will act synergistically.
Advertisement
“We’re very excited about the possibilities, but there’s still a lot to do,” says Dr. Keri. “We need to figure out why the tumors are particularly sensitive to that combination of therapies, so we are doing many different genomic studies to pinpoint the mechanism that makes cells particularly sensitive to paclitaxel when YES1 is inhibited.”
The Cleveland Clinic team plans on continuing to test this combined treatment in different mouse models, eventually moving on to studies with patient-derived xenografts. Another important goal is to develop a more selective YES1 inhibitor in collaboration with medicinal chemists and identify potential predictive biomarkers for this novel therapeutic approach.
Advertisement
Advertisement
First full characterization of kidney microbiome unlocks potential to prevent kidney stones
Researchers identify potential path to retaining chemo sensitivity
Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time
Investigators are developing a deep learning model to predict health outcomes in ICUs.
Preclinical work promises large-scale data with minimal bias to inform development of clinical tests
Cleveland Clinic researchers pursue answers on basic science and clinical fronts
Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches
Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology