Program reduces major contour changes and variations in organ-at-risk dosing across health system
A Cleveland Clinic-led analysis shows that subspecialty-led peer review for head and neck cancer can improve consistency and quality of radiation treatments plans across a large integrated health system. The results were presented at the 2025 annual meeting of the American Society for Radiation Oncology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In the past, Cleveland Clinic physicians reviewed cases during “chart rounds,” which took place during the week a patient began treatment. But as Jenna Kocsis, MD, radiation oncology resident at Cleveland Clinic Cancer Institute and lead author of the study, explains, that timing can create challenges.
“Chart rounds happen at some point during the week treatment starts, so if significant changes are identified, you may have to delay therapy or the patient may have already started,” she says. “Our goal with prospective peer review is to evaluate contours and plans about a week beforehand so we can ensure accuracy and avoid last-minute disruptions.”
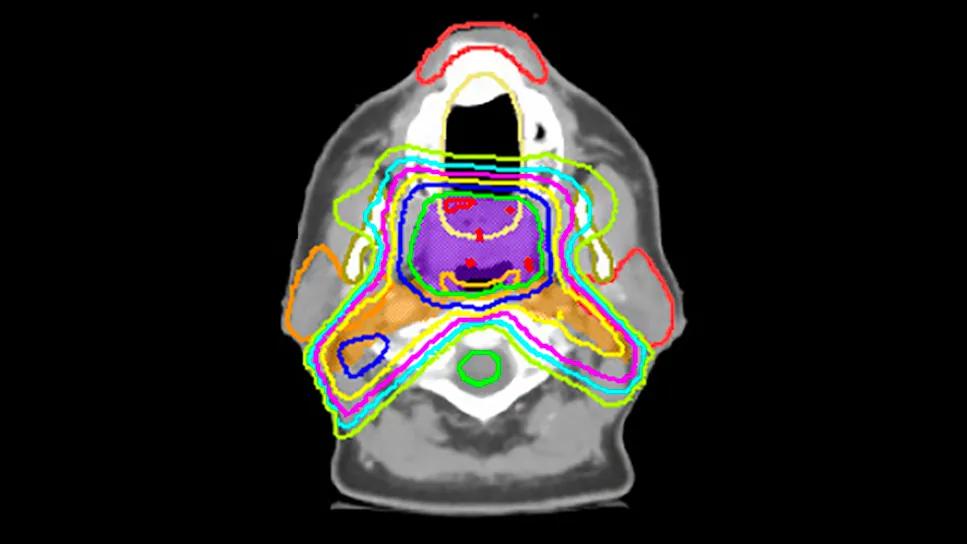
This approach is especially critical in head and neck cancer, where the anatomy is complex and small variations in contouring can lead to significant differences in dosages to critical structures. Prior studies at other institutions show that 40 percent or more of contours in large networks are modified during peer review, underscoring the challenge.
In 2018, Cleveland Clinic instituted a dedicated head and neck subspecialty (HNSS) peer review program. Centralized subspecialists began reviewing contours and plans not only from their own site but also from regional campuses across the health system. In 2023, the team launched a standardized database to track cases, recording how often changes were recommended and whether they were considered major or minor.
The current analysis reviewed 467 cases from 2023 to 2024. Regional campus physicians submitted 314 cases, while HNSS physicians submitted 153. Overall, recommended contour changes for regional cases significantly decreased over the two years. Additionally, there was an improvement at the individual physician level, with significant decreases in modifications over the same interval.
Advertisement
To evaluate whether these peer review sessions translated into objective improvements, the researchers analyzed dosimetry for oropharynx cancer cases treated with 70 Gy and elective 56 Gy to bilateral necks at three time points: 2018, 2021 and 2024.
In 2018, four of six organs at risk (OARs), although planned in a safe and effective manner, received significantly higher doses when comparing regional plans with HNSS cases. By 2024, only one structure remained significantly different, and median OAR doses at regional campuses improved by 5 to 25 percent compared with 2018.
“Head and neck peer review clearly improved radiation treatment plans over time,” says Shauna Campbell, DO, senior author of the abstract and staff radiation oncologist at Cleveland Clinic. “These findings provide objective evidence that peer review is not just a theoretical exercise — it makes a measurable difference in patient care.”
Beyond dosimetry, a survey of the physicians involved demonstrated an increased confidence in treatment decisions among general radiation oncologists. Seventy percent of respondents felt their ability to treat head and neck patients improved after attending peer review, and all respondents described the experience as positive.
“It’s about building consensus,” Dr. Kocsis notes. “Radiation is both art and science — dose prescriptions may be similar, but target volumes can be subjective. These meetings allow us to come together and agree on what we think is the right way to treat patients, so care is consistent across the network.”
Advertisement
Implementing such a program is not without challenges. Weekly sessions require significant administrative support, time away from patient care and dedicated communication among peers. At Cleveland Clinic, the solution was to dedicate one hour over lunch each week, with regional planners and dosimetrists attending virtually alongside subspecialists.
“It requires buy-in from specialists and a culture where feedback is seen as constructive,” Dr. Kocsis emphasizes. “But the payoff is standardized, higher-quality care.”
Given the success in head and neck cancer, Cleveland Clinic has recently expanded subspecialty-led peer review to other disease sites, including central nervous system, breast and gastrointestinal cancers.
“Head and neck was the logical place to start, given its complexity,” Dr. Campbell says. “But we believe this model can be adapted across disease sites to raise the standard of care across all locations.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors