Two large studies of virtual visits hold insights for post-pandemic practice

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/65b8f164-e301-49ed-96e7-7e2d667716cc/Artboard-1-100_jpg)
Artboard 1-100
In the year or so before the COVID-19 pandemic catapulted telemedicine to the forefront of outpatient practice across much of the world, clinicians in Cleveland Clinic’s Neurological Institute were reporting and analyzing data on some of the most widespread applications of teleneurology in the U.S.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
First came a plenary presentation at the 2019 annual meeting of the American Academy of Neurology (AAN), which represented the largest reported single-center experience with outpatient subspecialty teleneurology up to that point. Now staff from Cleveland Clinic’s Epilepsy Center have published in Epilepsia (Epub 22 July 2020; doi.org/10.1111/epi.16619) a report of the largest single-center experience implementing tele-epilepsy care to date, drawing on data from January 2017 to November 2019.
“Both studies demonstrate that large-scale implementation of teleneurology is feasible and associated with high levels of patient and provider satisfaction,” says Marisa McGinley, DO, a neurologist with Cleveland Clinic’s Mellen Center for Multiple Sclerosis and a co-investigator for both studies. “At Cleveland Clinic, we’ve recognized for several years that virtual visits can enhance patient access to subspecialized neurological care beyond just the well-established use of teleneurology in acute stroke care. This recognition led us to start offering at-home virtual visits across our Neurological Institute more than five years ago.”
This long-standing experience helped the Neurological Institute swiftly convert nearly all outpatient appointments to virtual visits in the early days of the COVID-19 outbreak, resulting in a 533% increase in teleneurology visit volume in the three weeks following March 15, 2020, as Dr. McGinley and colleagues reported in Telemedicine and E-Health (Epub 16 Jun 2020; doi.org/10.1089/tmj.2020.0137). “Our long experience has also yielded some large-scale data on teleneurology that can help inform how to make the most of virtual visits for subspecialized neurology care in the new telemedicine landscape brought about by the pandemic,” Dr. McGinley adds.
Advertisement
The Neurological Institute’s initial experience with subspecialty teleneurology was described in the pre-pandemic setting of the 2019 AAN annual meeting and published in full in Telemedicine and E-Health (Epub 23 Jun 2020; doi.org/10.1089/tmj.2020.0032). Using a cross-sectional study design, researchers identified all outpatient virtual neurologic follow-up visits — i.e., those conducted on a personal device videoconferencing platform — at Cleveland Clinic over a four-year period.
Overall, 5,581 virtual visits were completed among 3,913 unique patients. Mean patient age was 49.4 years, and 58.7% of patients were female. Virtual visits were completed in all of the Neurological Institute’s outpatient neurologic subspecialties, with visits for headache, epilepsy and spine care leading the pack. The annual number of virtual visits grew dramatically during the study period, from 30 in year 1 to 4,468 in year 4.
Virtual visits were used by patients both near to and far from Cleveland Clinic, as follows:
Patients rated their satisfaction with their overall virtual visit experience at a mean of 4.7 on a scale of 1 to 5; patients’ mean satisfaction with their provider was 4.9.
“This study demonstrates the feasibility of implementing outpatient teleneurology services across a wide range of subspecialties,” says Dr. McGinley. “Virtual visits resulted in high levels of patient satisfaction and significantly reduced patient travel — we calculated that 1.3 million miles of travel were avoided across the 5,581 visits. At the same time, the substantial proportion of virtual visits completed by local patients suggests that teleneurology can offer benefits and improve access for patients in ways that go beyond mere travel distance.”
Advertisement
Dr. McGinley subsequently joined colleagues from Cleveland Clinic’s Epilepsy Center to take a deeper dive into virtual visits specifically among patients with epilepsy in an even more recent study period.
“At the start of 2017, all patients in our tertiary care academic epilepsy center were given the opportunity to complete outpatient follow-up visits via videoconferencing using personal devices,” explains Jessica Fesler, MD, a staff physician in the Epilepsy Center and lead author of the resulting study in Epilepsia. For that study, she and colleagues retrospectively reviewed data for all epilepsy patients who self-selected these virtual visits from January 2017 to November 2019 — 3,698 visits in all among 2,140 unique patients.
The table below presents their key numeric findings in terms of patient data, visit data and the tele-epilepsy experience.
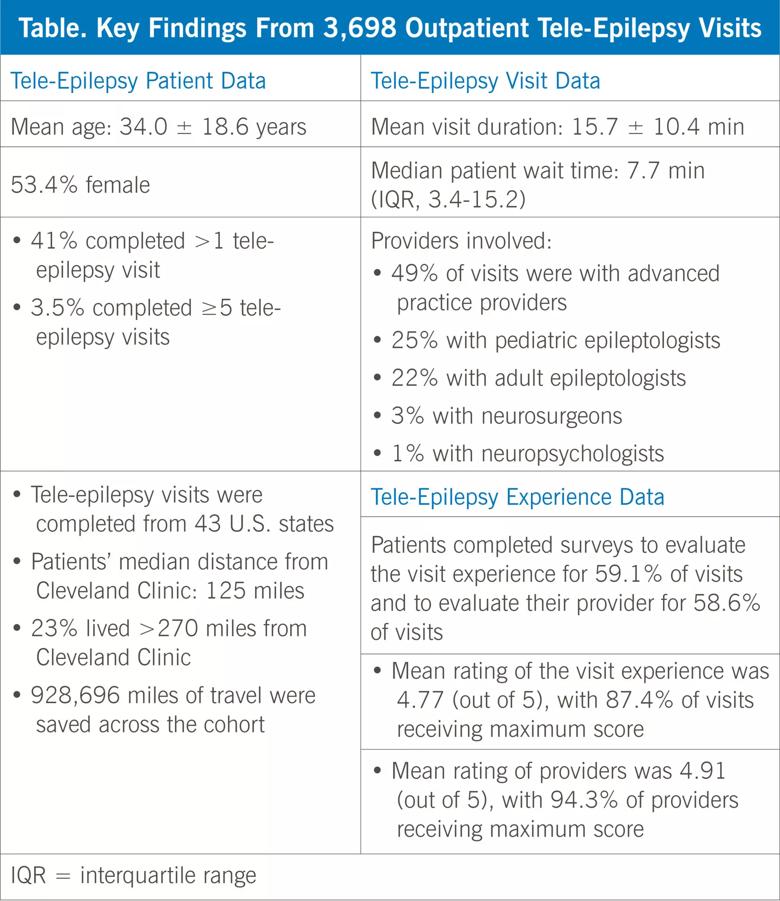
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d63d8434-2998-465c-8b10-0a137cc5efee/20-NEU-1917433-inset-scaled_jpg)
The researchers noted other significant observations, including the following:
Advertisement
“Collectively, these findings show that our large-scale implementation of tele-epilepsy for follow-up care was an overwhelmingly positive experience for patients with epilepsy from near and far,” says Dr. Fesler. “These results also demonstrate that tele-epilepsy is scalable, with the latter point underscored by our ability to convert our outpatient clinics — with almost 600 visits per week — to nearly a 100% tele-epilepsy practice during the first two weeks of pandemic lockdown.”
In their study report, Dr. Fesler and co-authors note that epilepsy care may be especially well suited to virtual visits, for a number of reasons:
At the same time, the researchers concede that current limitations of most forms of tele-epilepsy preclude its use when neuroimaging, EEG and other modalities are required. Indeed, they identify investigation into the best contexts for tele-epilepsy application, as well as its impact on healthcare delivery costs, as essential future research questions.
Advertisement
“Despite these pending questions and uncertainty about regulatory and reimbursement issues around virtual visits after the pandemic subsides, it looks like the future will favor rather than impede the telemedicine model for epilepsy and other neurological diseases,” concludes Dr. McGinley. “Our studies show how feasible it is as an alternative and/or supplement to traditional outpatient follow-up care.”
Advertisement
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology
Recommendations on identifying and managing neurodevelopmental and related challenges
Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies