Series demonstrates comparable results with an MRI-based decision strategy
Selecting children with epileptic spasms for surgery based on the location and extent of lesions detected on brain MRI, nearby eloquent regions and preexisting deficits yields seizure-free results comparable to a strategy that includes intracranial monitoring. This MRI-based approach not only reduces risk by avoiding an invasive procedure but allows surgery to be conducted more promptly. So concludes a study — recently published in Epilepsy Research — of a large series of children who underwent surgery for epileptic spasms without invasive monitoring.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“In prior surgical series of children with epileptic spasms, invasive intracranial EEG monitoring has been used in 20% to 65% of patients,” says the study’s corresponding author, Ahsan N.V. Moosa, MD, a Cleveland Clinic pediatric epileptologist. “At Cleveland Clinic, almost all children who have epileptic spasms with an epileptogenic lesion on MRI undergo surgery without invasive intracranial EEG monitoring. This series confirms that this approach is sound.”
Drug-resistant epileptic spasms in children may have a surgically remediable cause, Dr. Moosa notes. Most surgical candidates have an epileptogenic lesion detectable on brain MRI, but often they also have generalized features in semiology and on interictal and ictal EEG, which confuses the picture. The apparent nonlocalized epileptogenic pattern leads some clinicians to seek further data from intracranial EEG monitoring, with either subdural grid and depth electrodes or stereoelectroencephalography (SEEG). But these procedures entail risks of hemorrhage and infection, and their utility in the setting of epileptic spasms is uncertain.
“Observations from such studies have shown that the seizures were determined to arise from and around the lesion detected on MRI,” Dr. Moosa explains. “Therefore, the utility of intracranial EEG monitoring in this setting is unclear.” He adds that children younger than 2 years are generally excluded from SEEG because of potential complications related to the thin skull in these young patients. This may delay epilepsy surgery if SEEG is deemed necessary.
Advertisement
Evidence indicates, however, that delaying treatment in children with epileptic spasms, even by a few weeks, can have detrimental impacts on development. The American Academy of Neurology recommends initiating therapy within a week of onset of newly diagnosed epileptic spasms.
The retrospective study included 70 children with drug-resistant active epileptic spasms (in clusters or sporadic) who underwent surgical resection at Cleveland Clinic between 2000 and 2018. All were under 5 years old (mean age at seizure onset, 6.8 months; median age at surgery, 18.5 months). None underwent intracranial EEG.
All patients had an epileptogenic lesion identified by brain MRI. Seventeen (24%) had bilateral abnormalities that in all cases were strikingly asymmetric and worse on the side of surgery.
Spasms were the predominant seizure type in all patients and were the exclusive seizure type in 32. Sixteen children had additional seizures with focal features on EEG or semiology; other seizure types included generalized tonic-clonic seizures (n = 10), nonmotor seizures with behavioral arrest (n = 12) and myoclonic-atonic seizures (n = 2). Preoperative EEG showed hypsarrhythmia in 56% (39/70).
Etiologies were malformations of cortical development (58%), perinatal infarct/encephalomalacia (39%) and tumor (3%). Surgical procedures were hemispherectomy (44%), lobectomy/lesionectomy (33%) and multilobar resections (23%).
Outcomes were as follows:
Advertisement
Favorable outcomes at six months were associated with:
Increased risk of recurrence was associated with:
Dr. Moosa explains that Cleveland Clinic’s approach to epileptic spasms is to base surgical decisions primarily on the lesion detected on MRI. “The lesions are generally lobar or hemispheric,” he says. “When MRI abnormalities are bilateral, focal features on EEG and seizure semiology have guided surgical decisions.” The type and extent of procedure are influenced by preexisting deficits and anatomic margins of nearby eloquent cortex. Children with symmetrical extensive abnormalities on brain MRI are generally not considered to be surgical candidates, he notes.
He highlights key takeaways from his team’s analysis of this “MRI-based” approach:
Advertisement
“Not requiring invasive monitoring for epileptic spasms offers a faster path to surgery and exposes children to less preoperative risk,” Dr. Moosa observes. “It also opens up the availability of effective treatment in centers without intracranial monitoring capabilities.”
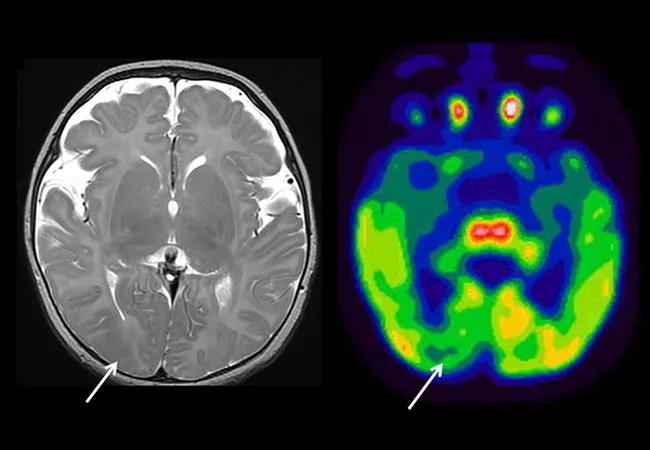
Image at top shows T2-weighted MRI and FDG-PET images from a 3-month-old infant with epileptic spasms and focal seizures. Arrows indicate focal areas of hypointensity and hypometabolism consistent with focal cortical dysplasia.
Advertisement
Advertisement

An argument for clarifying the nomenclature

An expert talks through the benefits, limits and unresolved questions of an evolving technology

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits