Two new studies add insights and home in on therapeutic targets

Two new human studies from a Cleveland Clinic research team led by Stanley Hazen, MD, PhD, have yielded additional insights into why and how regular consumption of red meat can increase the risk of cardiovascular disease (CVD) and the role that gut bacteria play in the process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
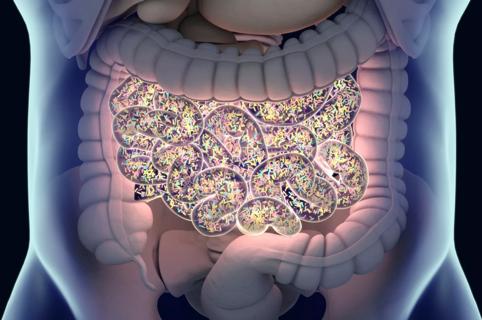
The studies — published online December 10 by the European Heart Journal and the Journal of Clinical Investigation — build on previous work by Dr. Hazen’s team and others showing that the metabolite TMAO (trimethylamine N-oxide) — a gut bacteria byproduct generated during digestion — is mechanistically linked to the pathogenesis of atherosclerotic heart disease. TMAO is produced when gut bacteria digest choline, carnitine and lecithin — nutrients that are abundant in animal products, particularly red meat. (TMAO’s linkages to CVD have previously been covered on Consult QD, including here and here.)
“These studies bring us closer to therapeutic interventions to reduce CVD risk in humans by reducing TMAO levels through diet manipulation or novel therapies targeted at specific steps in TMAO’s metaorganismal pathway,” says Dr. Hazen, Chair of the Department of Cellular and Molecular Medicine and Co-Section Head of Preventive Cardiology at Cleveland Clinic.
The investigation published by the European Heart Journal was a dietary intervention study assessing the impact of chronic dietary patterns on TMAO levels, metabolism and renal excretion. One hundred thirteen healthy adult volunteers were sequentially given four-week isocaloric meal plans prepared using either red meat, white meat or non-meat (mostly vegetarian) protein sources as 25 percent of daily calories. All participants also received a washout diet for at least two weeks between each of the monthly meal plans.
Advertisement
Results showed that chronic ingestion of red meat increased plasma levels of TMAO approximately threefold compared with consumption of white meat or non-meat protein (P < .0001), with some participants demonstrating increases of more than tenfold. Similar significant increases in urine levels of TMAO were observed during the red meat diet (P < .0001).
After discontinuation of the red meat diet, plasma TMAO levels subsided within four weeks.
Red meat consumption also significantly decreased fractional renal excretion of TMAO (P < .05) but increased fractional renal excretion of carnitine and two other gut microbiota-produced metabolites of carnitine: gamma-butyrobetaine and crotonobetaine (P < .05). “This is the first study, to our knowledge, to show that the kidneys can change how effectively they excrete different compounds — other than salts and water — depending on the diet consumed,” observes Dr. Hazen.
In a subgroup of participants given oral isotope tracers, isotope challenge showed that red meat and white meat — but not non-meat protein — significantly increased gut microbiota production of TMAO and its precursor TMA from carnitine but not from choline.
Dietary levels of saturated fat (low vs. high) were also examined across the study with each of the diets (red meat, white meat and non-meat protein) and were found to have no impact on TMAO or its metabolites.
“These findings add substantially to our understanding of diet and TMAO metabolism,” says Dr. Hazen. “In view of the growing body of evidence supporting a mechanistic link between TMAO and CVD pathogenesis, interest in TMAO-reducing therapeutic interventions is mounting. This study begins to provide evidence-based results regarding dietary manipulations that can effectively lower TMAO levels.”
Advertisement
The other new study from Dr. Hazen’s team, published in the Journal of Clinical Investigation, aimed to define the contribution of one of the abovementioned metabolites of carnitine, gamma-butyrobetaine (gamma-BB), in gut microbiota-dependent L-carnitine metabolism in humans in light of evidence that L-carnitine accelerates atherosclerosis in mice via TMAO formation in the gut.
The work was propelled by findings Dr. Hazen’s team published earlier this year in Nature Medicine showing that a new drug class developed by Cleveland Clinic researchers reduced platelet hyperresponsiveness and thrombosis potential in a mouse model without increased bleeding risk. The novel drug class acts by nonlethally targeting the gut microbial pathway that produces TMAO.
“Preclinical studies indicate that therapeutic targeting of microbial contributors to the TMAO pathway may hold promise for preventing or treating CVD,” Dr. Hazen explains. “But an improved understanding of the microbial pathways involved in TMA and TMAO formation from distinct nutrients in humans is a necessary step in the development of targeted therapies to disrupt these processes.”
To that end, the new study in the Journal of Clinical Investigation compared the impact of chronic daily oral carnitine supplements in omnivores versus vegans/vegetarians. At baseline, vegans/vegetarians showed virtually no ability to produce TMAO from carnitine, whereas omnivores rapidly produced TMAO. After one month of supplementation, both groups showed an increased capacity to produce TMAO, though vegans/vegetarians still produced decreased amounts relative to omnivores.
Advertisement
The researchers found that carnitine is converted to TMAO in the gut through a two-step process facilitated by distinct gut bacteria. The first step — rapid generation of the atherogenic intermediate metabolite gamma-BB — is similar in omnivores and vegans/vegetarians. But the second step — gamma-BB transformation into TMA — is significantly enhanced in omnivores (i.e., by the chronic dietary exposure found in an omnivorous versus a vegetarian diet). The researchers demonstrated that a daily carnitine supplement can induce TMAO production, even in vegans and vegetarians who continue consuming their usual diets. They also isolated and identified human gut commensals from fecal samples that could support each step in the overall transformation of carnitine to TMA/TMAO.
“We showed that gut microbial transformation of gamma-BB into TMA and then TMAO is induced by omnivorous dietary patterns and chronic carnitine exposure,” notes Dr. Hazen. “These findings provide important insights for efforts to develop therapeutic interventions to inhibit dietary conversion of carnitine into TMAO in humans.”
Advertisement
Advertisement

First full characterization of kidney microbiome unlocks potential to prevent kidney stones

Researchers identify potential path to retaining chemo sensitivity
Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests

Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology