Simulation educates nurses on intake and output
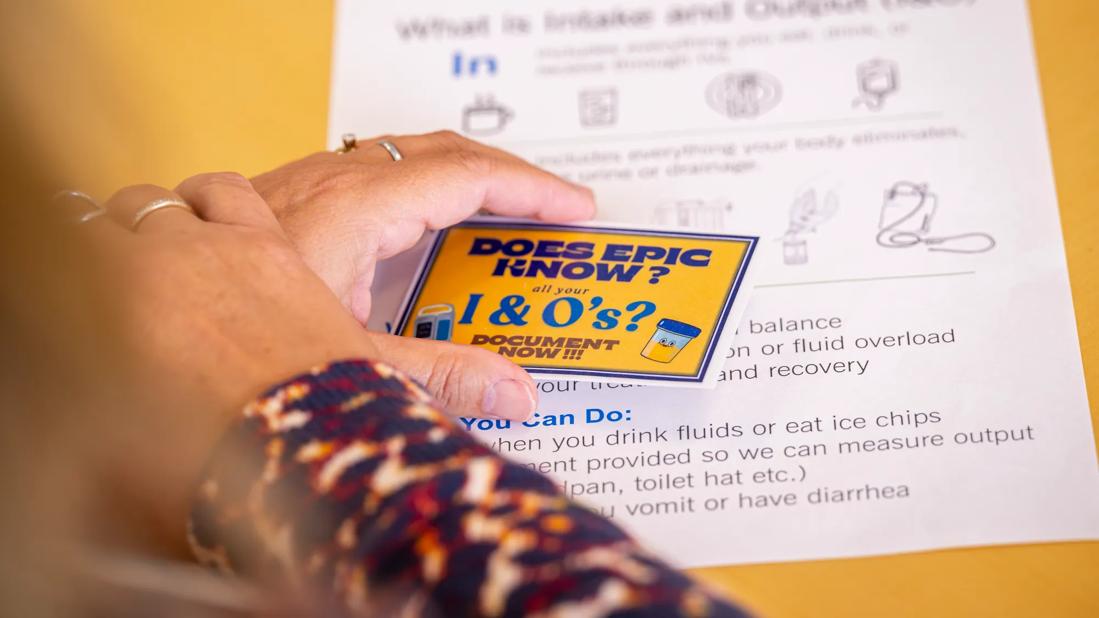
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8d3fc355-d316-400d-9c64-65e3e21ef40e/NUR_6759208_09-19-25_008_SCG)
Nursing paperwork
When nursing leaders saw documentation of patient intake and output (I&Os) dip to 60 percent on a busy medical-surgical unit at Cleveland Clinic’s Fairview Hospital, they took action. “While measuring and documenting I&Os is a basic essential function, sometimes in the complex world of technology and pharmacology we have competing priorities,” says Kathleen Singleton, MSN, APRN-CNS, CMSRN, a clinical nurse specialist for medical-surgical nursing. “Unfortunately, they fall off the radar.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Accurate measurement and documentation of I&Os are important because medications, intravenous and fluid administration, dietary decisions and tube feeding physician orders are based on I&O 24-hour totals. The numbers provide real-time data that guides daily care of the patient.
Singleton teamed with four other nurses, including Christine Wichert, MSN, APRN, CMSRN, GCNS-BC, assistant nurse manager on Fairview’s Parkview 3 med-surg unit, to create a simulation station to educate caregivers about the importance of I&Os and improve consistency in measurements in post-operative surgical patient populations.
Parkview 3 is a 36-bed med-surg unit with a mix of patients. “Nurses accept patients from several venues, so there are always patients arriving and leaving with varying levels of care that change rather rapidly,” says Singleton. “The medical-surgical nurse takes care of acutely ill patients, chronically ill patients and acutely-chronically ill patients simultaneously and can care for six to eight patients at any given time.”
Having a mix of patients presents challenges to obtaining I&Os. For instance, nurses may have one patient with congestive heart failure who is on restricted fluids, while another bariatric surgery patient is required to consume a certain amount of fluids per hour.
Another barrier to accurate I&O measurement relates to the med-surg environment itself: Patients can order their own meal trays, and visitors can bring them food. “With 24-hour visiting, that can go on all the time,” says Singleton. “So a lot of people aside from caregivers affect the patient’s accessibility to fluids and food.”
Advertisement
Singleton and Wichert created an I&O simulation center with input from Parkview 3 staff. “There are traditional mini-meetings, hand-outs and one-on-one in-servicing, but we wanted to do something that would grab people’s attention,” says Singleton.
The simulation station was on display for two weeks in a conference room on the nursing unit. The display included several common containers, including milk cartons, soda cans and Jell-O® cartons. Singleton and Wichert also made and displayed solutions to mimic output – urine, bile and emesis. In addition, there were hand-outs that explained the “ins and outs of I&O,” such as why it’s important, what patients need I&O measurements, who is responsible for measurements and documentation, and when it should occur.
The nurses who developed the simulation held 10 interactive sessions for registered nurses and patient care nursing assistants. They encouraged caregivers to pick up and examine the containers. They also gave a true/false quiz to participants, using some of these statements:
In addition, the team asked participants how much intake they would record for various fluids, including ice cream, a cup of coffee and Jell-O. Similarly, caregivers were asked to hold the faux output containers at eye level and indicate how they would record both urine and emesis.
Advertisement
Fifty-two caregivers from all shifts on Parkview 3 participated in the simulation. The med-surg unit experienced a 50 percent increase in obtaining I&Os in the month following the simulation station. In the quarter following the program, caregivers met or exceeded a target goal of 90 percent documentation three out of four months.
Wichert says caregivers continue to be vigilant, in part due to changing patient populations. “We’ve had a rise in colorectal surgeries and gastric bypass surgeries, so I think nurses are more aware that we need accurate I&Os to decide if patients can be discharged,” she says.
While measuring I&Os may seem like a basic task, it’s a vital one. “Obtaining and documenting accurate intake and output is a critical skill in providing safe care to surgical patients,” says Singleton. “Simulation was an engaging, fun and practical methodology to revisit basic care.”
Advertisement
Advertisement
Plastic surgery nurses uniquely help patients meet medical, functional and aesthetic goals
Strengthening outcomes through clear, transparent communication
Harnessing digital innovations to enhance nurse confidence and clinical outcomes
Regional organizations collaborate to address nurse faculty shortage
How wellness habits help nurses flourish
Planning continues with critical, patient-focused input from nursing teams
Strengthening care through targeted resources and frontline voices
Embracing generational differences to create strong nursing teams