Higher complete reperfusion rate seen with tenecteplase vs. alteplase in single-center study of stroke with LVO
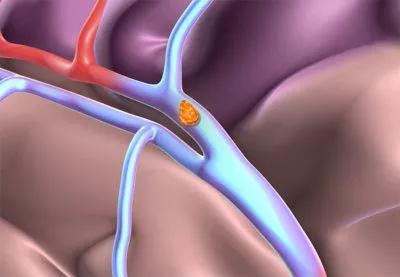
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/91c0a2c4-ac52-4ad0-aea6-5a722cae718f/23-NEU-4479131-thrombolysis-ischemic-stroke-650x450-1_jpg)
23-NEU-4479131-thrombolysis-ischemic-stroke-650×450
Tenecteplase (TNK) is associated with a higher rate of TICI 3 recanalization than alteplase (tissue plasminogen activator; tPA) in stroke patients with large vessel occlusion (LVO) who receive thrombolysis and mechanical thrombectomy. So finds a retrospective Cleveland Clinic study presented at the 2024 International Stroke Conference (ISC 2024).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This higher rate of complete reperfusion in stroke patients undergoing thrombectomy was achieved despite an absence of significant differences between TNK and tPA in regard to the number of passes, time to recanalization, hemorrhage rates and clinical outcomes,” notes study co-author and Cleveland Clinic interventional neurologist Gabor Toth, MD.
A bioengineered tissue plasminogen activator and thrombolytic agent, TNK has been proven to increase reperfusion and functional outcomes in patients with acute ischemic stroke. The current study was undertaken to explore whether TNK’s increased specificity for fibrin relative to tPA might translate into better outcomes in a subset of that population undergoing mechanical thrombectomy due to underlying LVO.
The researchers reviewed data from adults presenting with acute LVO stroke at Cleveland Clinic’s Comprehensive Stroke Center from January 2017 to April 2023. Only patients who received thrombolysis (with either TNK or tPA) and underwent mechanical thrombectomy were included. Number of passes and time to full recanalization — defined as Thrombolysis in Cerebral Infarction grade 3 (TICI 3) — were recorded.
The primary outcome was modified Rankin scale (mRS) score at 90 days. Secondary outcomes were National Institutes of Health Stroke Scale (NIHSS) scores at 24 hours and at discharge. The primary safety outcome was parenchymal hematoma type 2 (PH2) intracerebral hemorrhage.
“We looked at the number of passes and recanalization time as surrogate markers for drug efficacy in this population, and hemorrhage as a surrogate marker for safety,” Dr. Toth explains.
Advertisement
Associations between outcomes and thrombolysis type were statistically analyzed, as were differences in rates of recanalization and hemorrhage with TNK versus tPA.
Preintervention characteristics of the two treatment groups were comparable (mean age of 68; 50% female), but more patients received tPA (n = 213) than TNK (n = 71).
“Fewer patients received TNK than tPA because TNK did not become standard of care for thrombolysis in adults with acute ischemic stroke at Cleveland Clinic until early 2022,” says Dr. Toth. “This study represents approximately 1.5 years of experience with TNK versus five years with tPA.” Cleveland Clinic was a relatively early adopter of TNK for acute stroke thrombolysis on an enterprise-wide basis when it made the switch from tPA in January 2022, based on evidence from clinical trials and guidelines as well as the experience of other health systems.
Complete reperfusion — a score of 3 on the TICI scale of 0 to 3 — was achieved in 43 patients who received TNK (60.6%) versus 96 patients who received tPA (45.1%) — a significant difference (P = 0.028).
“Increased recanalization rates seen with TNK in our analysis appear to correspond with previous studies showing higher fibrin specificity with TNK and greater resistance to plasminogen activator inhibitor-1, likely resulting in higher efficacy,” notes co-author and Cleveland Clinic neurology resident Aron Gedansky, MD. “This appears to further support the use of TNK.”
Among patients in both groups who achieved TICI 3 recanalization, time to that outcome did not differ between the groups (38.5 vs. 32 minutes with TNK and tPA, respectively; P = 0.872). There also were no between-group differences in median number of passes (1 vs. 1), median 90-day mRS score (2 with TNK vs. 1.5 with tPA; P = 0.434) or rate of PH2 hemorrhage (0% vs 2.3%, respectively; P = 0.336).
Advertisement
Similarly, median NIHSS scores did not differ between the TNK and tPA groups at any of the time points studied — presentation, 24 hours or discharge.
“We were hoping to see major differences between TNK and tPA with regard to clinical outcomes, especially with higher recanalization rates with TNK,” Dr. Toth notes. “We think that a larger study may have more power to achieve that goal, but the overall efficacy and safety of TNK has been well demonstrated by our experience with the drug at Cleveland Clinic over the past two years. A multicenter study in a larger population may be needed to elicit further trends in outcomes and safety with TNK versus other thrombolytics in patients undergoing mechanical thrombectomy.”
Advertisement
Advertisement
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Aim is for use with clinician oversight to make screening safer and more efficient
Tasked-based therapy improves social connection and quality of life
LAA closure may be compelling option in atrial fibrillation ablation patients at high risk of both stroke and bleeding
Case illustrates essentials of the low-risk, high-potential procedure when paired with rehab
New analyses confirm preservation of ablation outcomes, broaden data on bleeding benefits
Increasing treatment options are extending the window for continued functional gains
Findings help close the knowledge gap around VTE practice patterns