Our Cancer Center Chair reflects on progress and potential

By Brian J. Bolwell, MD, FACP
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Two years ago, our print publication Cancer Advances featured an interview with me in which I discussed our efforts in reducing the time patients with cancer wait from diagnosis to treatment. I was pretty proud of the progress we’d made in 2017, but as I wrote then, “The work isn’t done.”
We haven’t slowed down our efforts; at that time, we were only beginning to understand the significance of time-to-treat (TTT) on patient outcomes. We were just beginning to see the benefits of our programs. Much has changed in two years.
What hasn’t changed is our core belief that reducing delays in TTT is the right thing to do. Cancer is associated with more fear than any other diagnosis, and that fear gets magnified the longer a patient and their family wait to begin treatment. We now have even more evidence that prolonged TTT may be associated with deleterious outcomes in certain cancers, including our most recent publication in PLoS Oneshowing that the absolute risk of mortality increases weekly for cancers like early-stage breast, lung, renal and pancreatic cancers.
And despite our significant progress, we still consider TTT a top priority for our cancer center. I think the time it takes for a person to receive their first therapy after diagnosis is a surrogate marker for the amount of empathy in a culture. Time-to-treat is now simply part of our patient-oriented culture, and it’s embedded into our cancer programming model that brings together clinicians by disease, not by department.
Advertisement
What has changed — and changed significantly — is our patients’ time-to-treatment. In 2017, we were proud to share that we’d cut about 10 days from our initial TTT average of 39 days. In a recent article in NEJM Catalyst, we reported a 33 percent reduction since the program began.
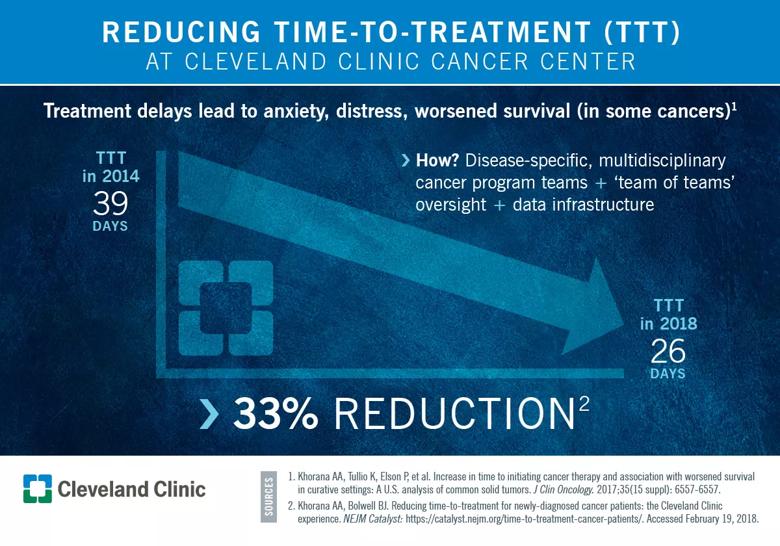
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/38542c60-9e72-494f-9dd6-f0615a85ec24/19-CNR-637-Visual-Abstract-v7_jpg)
I wrote in 2017 that our challenge wasn’t achieving the result, but maintaining it. It’s been two more years of hard work, but we’ve maintained our focus, which has resulted in this additional decrease in TTT.
We’ve also continued to eliminate outliers. When we started the process, about 30 percent of our patients had a TTT of more than 45 days, which is way too long. We want that number to be zero. We’ve reduced the proportion of all outliers from 30 to 14 percent, a 53 percent drop.
Another area of focus is patients who come to us from other institutions. We’ve done quite well reducing TTT in patients from within our own system, but sometimes weeks have gone by since a patient’s diagnosis before we are even notified that they need us. So one of our next big goals is to enhance our education to referring physicians, to emphasize the importance of getting their patients to us quickly, and to have the tools in place to see them right away.
The most significant change in the last two years has been in the national conversation on this issue. TTT is not a Cleveland Clinic issue; it’s a healthcare issue, and that’s becoming clear as we publish more data and show the benefits of getting cancer patients in faster. In fact, some national organizations are incorporating TTT as one of their quality metrics. That kind of widespread cultural change is something we couldn’t have achieved two years ago.
Advertisement
Finally, I don’t believe the only way to go from here is down in terms of number of days from diagnosis to treatment. We can’t just go on autopilot now that we’ve identified and addressed all the hurdles. The initial part of this process can be especially difficult, particularly in academic cancer centers, but this isn’t a problem that will go away anytime soon, as healthcare systems trend toward complexity and fragmentation. We’ll always need to pay close attention to TTT. It’s part of our culture, and it’s the right thing to do for our patients.
Dr. Bolwell is Chair of Cleveland Clinic Cancer Center.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient