International study supports change in clinical care in post-neoadjuvant setting
The antibody drug conjugate trastuzumab deruxtecan (TDXd) improves invasive disease-free survival (IDFS) by 53% over the current standard of care in patients with high-risk, HER2+ early breast cancer with residual invasive disease after neoadjuvant therapy, according to a global phase 3 study.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“These findings have the potential to bring a new adjuvant standard of treatment for high-risk HER2-positive breast cancer after neoadjuvant therapy,” says Jame Abraham, MD, Study Chair for NSABP and Chairman of the Department of Hematology and Medical Oncology at Cleveland Clinic Cancer Institute.
This is the first study which showed TDXd improved outcomes over trastuzumab emtansine (T-DM1) in the adjuvant setting after neoadjuvant therapy. The results of the DESTINY-Breast-05 trial were presented at a Presidential Symposium during the 2025 European Society for Medical Oncology (ESMO) Congress.
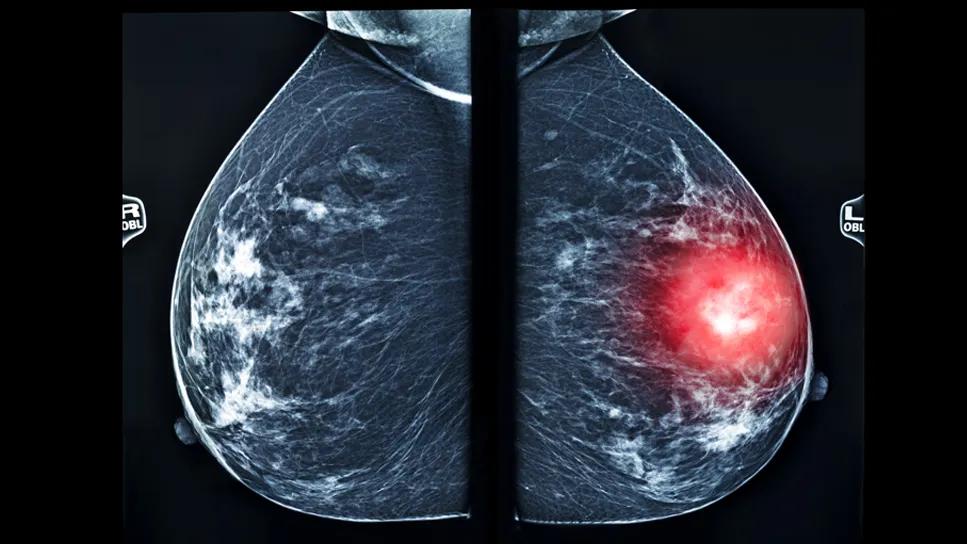
Breast cancer remains one of the leading causes of cancer-related deaths in women, and there is a pressing need for more effective treatments in the early stages of disease. Roughly a quarter of breast cancers are HER2+, which is associated with more aggressive disease and a higher chance of recurrence and mortality.
Nearly half of patients with HER2+ early breast cancer have residual disease after neoadjuvant therapy. The current standard of care when that occurs is administering the T-DM1 as adjuvant therapy in patients with residual disease after neoadjuvant therapy. Although TDXd and T-DM1 are both antibody drug conjugates, several studies have shown that TDXd is one of the most active HER2-targeted medicines.
The antibody drug conjugate (ADC) trastuzumab deruxtecan is composed of:
Advertisement
Together, this novel ADC eliminates target tumors cells as well as surrounding tumor cells. “The development of TDXd is one of the biggest advances in breast cancer treatment in recent years,” says Dr. Abraham. However, to date, there have been few studies examining its efficacy and safety in a head-to-head comparison with T-DM1, in the adjuvant setting.”
The DESTINY-BREAST-05 trial assessed patients from 400 different cancer centers across 33 countries to better understand efficacy rates and safety profiles in these two antibody drug conjugates.
To be eligible for the study, patients needed to meet the following criteria:
Of the 1,635 patients in the trial, 818 were randomized to T-DXd (5.4 mg/kg) and 817 were randomized to T-DM1 (3.6 mg/kg). The IV medications were administered once every three weeks for 14 cycles. The median age of patients was 50.3 years old in the T-DXd cohort and 50.6 years old in the T-DM1 cohort. The median study duration was 29.9 months with T-DXd and 29.7 months with T-DM1.
The primary endpoint was invasive disease-free survival (IDFS). The secondary endpoints were investigator-assessed disease-free survival, overall survival, distant recurrence-free interval, brain metastases-free interval and safety. In addition, the researchers assessed the risk of interstitial lung disease (ILD) through chest CTs during screening, after completion of radiation, prior to the first infusion and at regular intervals throughout treatment.
Advertisement
Outcomes revealed clinically meaningful benefits of TDXd over TDM-1. At three years, IDFS rates were 92.4% of patients in the TDXd arm and 83.7% of patients in the TDM1 arm (which is roughly a 53% improvement in IDFS with TDXd). In addition to reducing the risk of invasive disease recurrence or death by more than half, TDXd resulted in other numerous statistically significant improvements.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ccdcdeb3-61a9-4641-b004-1703d43bebfd/destiny-breast-trial-05-chart-inset)
“I'm really impressed by the magnitude of the benefit,” says Dr. Abraham. “These findings will potentially change the practice of treating early-stage, HER-2 positive breast cancer.”
The safety profile observed in this study was consistent with the known profile of the medication. In terms of Interstitial Lung Disease (ILD), 9.6% of patients receiving T-DXd and 1.6% of patients receiving T-DM1 experienced any grade ILD. Most ILD events were grade 1 or 2. In general, Dr. Abraham advises that patients receiving either therapy should be proactively screened and monitored for cardiac and lung issues and watched for symptoms such as a cough or shortness of breath.
The global research team will conduct longer follow-up to assess overall survival from the medication. In the future, they hope to continue to study T-DXd on earlier disease settings.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors