Cases of myalgia and arthralgia after CPI
By Moshe C. Ornstein, MD, MA, and Cassandra Calabrese, DO
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Immune checkpoint inhibitors (CPIs) have revolutionized the treatment of many cancers including genitourinary (GU) malignancies such as renal cell carcinoma (RCC) and urothelial carcinoma (UC). Unfortunately, the unleashed immune system not only battles malignancies; it also allows autoimmune diseases to flourish.
These diseases, known as CPI-induced immune-related adverse events (irAEs), can affect every organ system — from dermatologic to ophthalmologic, gastrointestinal, endocrine and others. Fortunately, many irAEs, including pneumonitis, colitis, hepatitis and endocrinopathies, have been well-characterized and can be treated quickly and appropriately. However, we don’t know as much about rheumatologic irAEs myalgia and arthralgia; thus, they have been harder to treat.
In 2016 our institution had established an interdisciplinary referral clinic with rheumatology and oncology to help manage a growing influx of patients with irAEs. By 2017, we had created a multidisciplinary monthly tumor board to discuss new and/or challenging cases of irAEs, review the extant literature and receive input on interprofessional management.
CPI-induced myalgia and arthralgia are two examples of challenging irAEs the board analyzes. Recently, we conducted a retrospective investigation of the clinical characteristics, treatment and outcomes of these two conditions that resulted interruption or discontinuation of CPIs in patients with GU malignancies.
We identified 21 patients, of which 18 had RCC and three had UC. Seventy-one percent were male, and the median age at diagnosis was 56 years. CPI therapy included antiprogrammed death-ligand 1 (29 percent), antiprogrammed cell death protein 1 (48 percent) and combined programmed cell death protein 1/cytotoxic T-lymphocyte-associated protein 4 antibodies (24 percent).
Advertisement
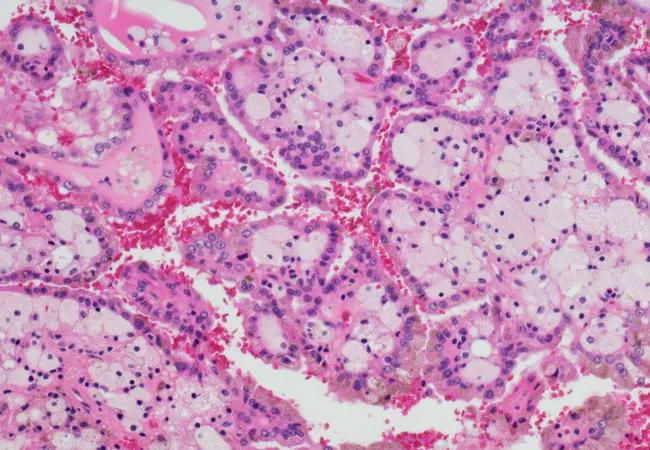
All patients with metastatic RCC had clear-cell histology and prior nephrectomy. Eight patients had a history of joint disease. Patients with mRCC and mUC had typical sites of metastases. Of the 21 patients, 13 had received systemic therapy prior to CPI, most (54 percent) patients with mRCC received antiangiogenic therapy prior to CPI, and one of the patients with mUC had previously received chemotherapy. The other two patients received CPI as front-line therapy.
The median time from the beginning of CPI therapy to the onset of myalgia and arthralgia irAEs was 5.1 months (range, 0.23 to 50.5 months). All patients were treated with prednisone with a median initial dose of 40 mg/d (range, 10-90 mg/d) for a median duration of 64 weeks (range, 3 to 242 weeks).Six patients were referred to rheumatologists for management and given prolonged steroid use with minimal symptom improvement. Five of these patients required treatment intensification with methotrexate, infliximab, tocilizumab, gabapentin and etanercept.
Six patients (29 percent) who ceased therapy due to irAEs restarted CPI therapy following symptom improvement, three (15 percent) switched to another therapy and 12 (55 percent) patients experienced an ongoing sustained response to therapy (median, 14.5 months; range, 3 to 55 months).
It’s challenging to characterize myalgia and arthralgia irAEs in a specific manner given their similar symptoms of bone and muscle pain. Standard assessments for synovial fluid and rheumatologic circulating antibodies are not performed on most patients, so we rely on more vague descriptions of number of joint groups involved, the presence of edema and symmetric versus asymmetric involvement.
Advertisement
Unfortunately, we’ve yet to prospectively validate and incorporate biomarkers into clinical practice for the prediction of irAEs. Our group does perform a panel of rheumatologic blood tests at baseline for patients with GU malignancies receiving CPI, including antidouble-stranded DNA,a n antinuclear antibody, rheumatoid factor, anti-extractable nuclear antigen, anti-citrullinated peptide antibody, erythrocyte sedimentation rate and c-reactive protein. This may help us delineate whether a patient’s pathology is driven by a rheumatologic or inflammatory process, which can affect treatment choices, such as the use of disease-modifying anti-rheumatic drugs and immunosuppressants.
Several analyses have proposed that the development of irAEs may be indicative of enhanced clinical efficacy and that CPI discontinuation does not result in poorer clinical outcomes. Our study also supports this evidence. Although we did not have a control arm, a relatively high percentage (55 percent) of patients whose development of myalgia and arthralgia required therapy discontinuation maintained disease stability (median, 14.5 months; range, three to 55 months), despite not receiving any subsequent anticancer therapy.
Overall, we recommend multidisciplinary teams that include a rheumatologist and oncologist for optimal patient management.
Dr. Ornstein is staff in the Department of Hematology and Medical Oncology. Dr. Calabrese is staff in the Department of Rheumatic and Immunologic Diseases.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient