Mounting evidence of possible shared genetic predisposition

A familial analysis using the Utah Population Database reveals evidence of familial aggregation of stiff-person spectrum disorder (SPSD) and other autoimmune conditions. The findings, presented at the 2023 annual meeting of the American Academy of Neurology by Cleveland Clinic neurologist Justin Abbatemarco, MD, bolster earlier evidence suggesting a clustering of autoimmune comorbidities within SPSD cohorts.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We found that patients with stiff-person spectrum disorder had higher rates of other autoimmune conditions, including type 1 diabetes, pernicious anemia and vitiligo, compared with controls,” says Dr. Abbatemarco, a staff physician with Cleveland Clinic’s Mellen Center for Multiple Sclerosis and former fellow at the University of Utah. “Clustering of these other autoimmune conditions occurred at a much higher rate than you would see in the general population, which supports the possibility of a shared genetic predisposition for these disorders.”
SPSD is a rare autoimmune disorder that causes progressive disability and has a variable response to immunotherapy. It encompasses classic stiff-person syndrome — characterized by fluctuating muscle spasms, severe gait instability, and exaggerated startle effect and anxiety — as well as variants that may involve just one limb, encephalopathy, and overlap syndromes such as temporal lobe epilepsy or cerebellar ataxia.
Prior investigations have detected clustering of other autoimmune conditions within SPSD cohorts that suggests some shared genetic predisposition. Indeed, studies in the past decade suggest that up to 60% of patients with SPSD are affected by an autoimmune disorder prior to or following onset of SPSD.
To further elucidate the genetic predisposition to SPSD, Dr. Abbatemarco and colleagues conducted a retrospective review of all patients with confirmed SPSD diagnosed and managed at the University of Utah’s autoimmune neurology clinic. They then developed estimates of familial risk and heritability of SPSD based on their analyses of genealogic records of more than 11 million people in the Utah Population Database (UPDB), which includes the relatively small group that founded Salt Lake City and modern communities in the greater Utah area.
Advertisement
“This is a unique database with extensive genealogical records for people of that area, combined with more recent medical and demographic information,” Dr. Abbatemarco explains. “It allows us to look for potential familial clustering and better target genetic testing and, ultimately, treatment for SPSD.”
The investigators identified high-risk pedigrees from the UPDB with excess familial aggregation of SPSD. Unaffected control subjects from the UPDB were identified and matched 10:1 with the University of Utah patients with confirmed SPSD; matching was done by age, birth year and pedigree structure.
The researchers identified 49 patients with SPSD. Patients were predominantly female (80%) and white (90%) and had a mean age of 52 years. Among this cohort, 51% had classical SPS and 34% had SPS overlapping with ataxia, epilepsy or encephalitis.
Antibody assays showed that 46 patients (95%) had glutamic acid decarboxylase (GAD65) antibodies, 11 (22%) had α1-subunit of the glycine receptor (GlyR) antibodies (eight with concomitant GAD65 antibodies) and one (2%) tested negative for all antibodies.
Compared to controls, patients with SPSD had significantly higher rates of type 1 diabetes (42.9% vs. 3.7%), thyroid disorders (49% vs. 23.5%), pernicious anemia (12.2% vs. 1.4%) and vitiligo (14.3% vs. 0.2%) (P < 0.01 for all).
The researchers found that the relative risk of SPSD in a pedigree in this cohort was significantly elevated compared with matched controls (P = 0.002).
“When we constructed multigenerational pedigrees going back generations, we could see familial clustering of these patients,” Dr. Abbatemarco says. “In particular, we identified four pedigrees in two distantly related families that both had SPSD. This provides additional impetus to do further genetic testing in this small population. The community in the Salt Lake City area was founded by a relatively small group of people, so patients may have distant relatives with SPSD that they may not be aware of.”
Advertisement
Awareness of this rare disorder has increased since the 2022 diagnosis of Canadian singer Celine Dion. “Patients usually present with a fluctuating course of muscle rigidity that may be painful,” Dr. Abbatemarco notes. “They often have axial or truncal spasms of the core abdominal muscles or back muscles, to the point where they can have hyper curvature of the lumbar spine, severe gait instability and severe anxiety around this disorder. It can sometimes lead to agoraphobia and fear of having the symptoms in social situations.”
Given the small and specific cohort studied, Dr. Abbatemarco cautions against generalizing his group’s findings. Further research is needed to facilitate targeted genetic testing in higher-risk individuals. “The University of Utah is now obtaining funding for such research,” he says. “We need to better understand the pathophysiology of SPSD so that we can target treatments for these patients and help them get their lives back.”
Advertisement
Advertisement

Heightened awareness of this rare disorder may lead to better diagnosis and treatment progress

Despite less overall volume loss than in MS and NMOSD, volumetric changes correlate with functional decline

It’s time to get familiar with this emerging demyelinating disorder

From dryness to diagnosis
Early experience with the agents confirms findings from clinical trials
Early data show risk is 73% higher in patients with lupus, 40% higher in patients with rheumatoid arthritis

Despite advancements, care for this rare autoimmune disease is too complex to go it alone
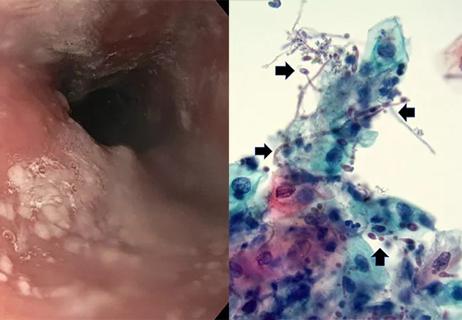
Treatment for scleroderma can sometimes cause esophageal symptoms